Veterans have given so much of their time, energy, and sacrifice in service to our country. Sometimes the simplest gestures can mean the most. Below are 11 meaningful ways to say “thank you” to a veteran — from personal acts of kindness to nationwide programs that make a real difference.
1. Write a Personal Thank-You Note
A handwritten letter or card expressing genuine appreciation can be incredibly meaningful. Mentioning specific freedoms or opportunities you’re thankful for personally goes a long way.
Tip: Organizations like A Million Thanks collect letters of gratitude and deliver them to active-duty service members and veterans.
2. Support Veteran-Owned Businesses
Shop at, dine in, or hire veteran-owned companies. Your purchases directly support veterans’ livelihoods.
Try: Use the Buy Veteran Directory from the National Veteran-Owned Business Association to find businesses near you.
3. Volunteer with a Veterans Organization
Offering your time can mean just as much as donating money. Check out Mission Roll Call’s Veteran Resource Directory to find trusted organizations to volunteer through.
4. Attend or Organize a Veterans Event
Show up at local or national ceremonies, parades, or community events on November 11 and throughout the year.
Find events: The U.S. Department of Veterans Affairs Events Calendar lists nationwide Veterans Day and remembrance gatherings.
5. Offer Your Skills or Services
If you’re a professional in finance, legal aid, healthcare, or home repair, offer free or discounted services to veterans.
Idea: Partner with Hire Heroes USA, which helps veterans transition to civilian careers.
6. Spend Time Listening
Invite a veteran for coffee or lunch and ask about their story — then truly listen. Sometimes the best “thank you” is genuine attention and respect.
7. Fly the American Flag Respectfully and Proudly
Displaying the flag properly, especially on Veterans Day, Memorial Day, and Independence Day, shows your pride and appreciation.
Learn more: The American Legion’s Flag Etiquette Guide explains how to display the flag correctly.
8. Support Veterans’ Mental Health Initiatives
Help break the stigma by supporting or advocating for programs that provide mental-health care for veterans.
Programs to support:
- Give an Hour – offers free mental-health services.
- Stop Soldier Suicide – provides crisis support and long-term care.
9. Invite a Veteran to Share Their Story at a School or Community Event
Sharing personal stories helps preserve history and fosters understanding across generations.
Resource: Nominate a veteran—or even yourself—to be honored on our platform. Share their story and help us celebrate their service and sacrifice.
10. Include Veterans in Everyday Community Activities
Inclusion is one of the simplest ways to show appreciation. Invite veterans to join neighborhood projects, book clubs, or volunteer efforts.
Organization spotlight: Team Rubicon engages veterans in disaster-response missions worldwide.
11. Say “Thank You for Your Service”
Never underestimate the power of a sincere “thank you.” When you meet a veteran, eye contact and gratitude can go a long way.
Conclusion
Every veteran’s story is unique, and so is the way they receive thanks. Whether you write a note, attend a parade, or simply say, “Thank you for your service,” every gesture matters. By supporting veteran-focused organizations and practicing everyday gratitude, we strengthen the bond between those who served and the nation they defended.
If this list inspired you, share it with friends or post it on social media this November. Encourage others to pick one of these 11 ways and act on it. Gratitude becomes more powerful when it’s shared — let’s keep saying “thank you,” not just in words, but in action.
Turn gratitude into action with Mission Roll Call. Saying “thank you” is powerful, but listening and acting alongside veterans is even more meaningful. Mission Roll Call gives every veteran a voice in shaping the policies and programs that impact their lives. When you join, you’re not just expressing gratitude — you’re helping ensure veterans are heard, valued, and supported long after their service ends.
Join the movement. Stand with those who served. Share your voice with MissionRollCall.org to get involved today.
Every year on November 11, our country pauses to honor the men and women who have served in uniform. But how did this day begin, and what makes it different from other military observances?
A moment rooted in world history
November 11 was originally known as Armistice Day. It marked the armistice that ended World War I on the eleventh hour of the eleventh day of the eleventh month in 1918. The guns finally went silent, and the modern era of veteran commemoration began.
In 1954, after World War II and the Korean War, Congress officially changed Armistice Day to Veterans Day to honor all who served. This includes service in times of war and peace, across every generation.
Veterans Day vs Memorial Day vs Armed Forces Day
These observances are often confused, but they each recognize something specific.
| Observance | When it’s observed | Who it honors |
| Memorial Day | Last Monday in May | Those who died in service to our nation |
| Armed Forces Day | Third Saturday in May | Those currently serving in the U.S. military |
| Veterans Day | November 11 | All who have served, past and present |
Veterans Day is a chance to thank the veterans around us for their service and their continued presence in our communities.
Why this day still matters
Veterans Day is more than a date. It’s a reminder that when military service ends, the journey does not. The transition home, the reintegration process, the need for timely care, meaningful purpose, and a strong support network continue long after the uniform is hung up.
Want to learn more?
Mission Roll Call University (MRCU) has a short video that walks through the history of Veterans Day and why this date has endured in our national story.
This Veterans Day, take a moment to thank a veteran in your life. A simple message of gratitude can mean more than you know. To all those who’ve answered the call, past and present, thank you for your service.
Every Veterans Day, businesses across the country show their appreciation for those who have served by offering special discounts, free meals, and other perks. Below are some of the top offers available to veterans, active-duty service members, and their families this year.
Before heading out: Most offers require proof of service (such as a military or veteran ID, DD-214, or verification through ID.me or SheerID). Participation can vary by location, so be sure to call ahead and confirm details.
We’ll continue updating this list as new deals are announced, so check back often for the latest ways companies are saying thank you.
A–Z Veterans Day Deals (2025)
A
- Abercrombie & Fitch — 10% off in-store purchases.
- Adidas — 30% off in-store & online; 20% off factory stores.
- Advance Auto Parts — 10% off regularly priced, in-store purchases for veterans, service members, and immediate family (ID required; exclusions apply).
- Alamo — Call 1-800-GO-ALAMO for government/military discounts.
- All Seasons Uniforms – This family-owned business, founded more than 30 years ago, offers a 10% discount for all military veterans on everything from corporate apparel to workwear. “It’s our way of saying thank you to the men and women who guarantee our freedom,” their team shared.
- Amanda Products — 10% military discount (year-round; proof of service).
- American Muscle Car Museum — Free Open House on Veterans Day for veterans, active duty, and families (not open to the public).
- Anthem Off-Road — 15% “Hero Discount” (email ID for custom link; includes certain fees/plan).
- Apple — 10% off select products.
- AT&T — 25% off select unlimited wireless plans (and other potential savings).
- Audi — Year-round Military Select Program: $1,000 toward eligible new vehicles (verify via ID.me).
- AutoAccessoriesGarage.com — Private military discount 5%–20% (veterans/active duty; email DD-214; extends to immediate family).
- Avis — Up to 35% off PAY NOW rates for Veterans Advantage members.
B
- Banana Republic — 10%–15% off in store (ID required).
- Bed Bath & Beyond — 25% off in-store on Nov. 11.
- Best Buy — Up to 10% (check local store).
- BMW — Military incentive $500–$5,000 on new leases/purchases (verify via ID.me).
- Bob Evans — Special free menu for veterans.
- Bonobos — 20% off for veterans, active duty & families.
- Brakes To Go — 10% off brake services (show military/veteran ID).
- Budget — Up to 35% off car rentals via Veterans Advantage (verification required).
- Buick — GM Military Program; combinable with most current offers (verify eligibility).
C
- Cadillac — GM Military Appreciation (active/reserve/NG/retirees/veterans/household). Register for authorization number.
- California Pizza Kitchen — Free meal + non-alcoholic drink Nov. 8–10; 20% of sales those days benefit DAV.
- CarParts.com — Discount for military members, veterans, and retirees.
- Casey’s — Free coffee Nov. 11; November donation on specific pizza + Pepsi bundle to veteran orgs.
- Chili’s Grill & Bar — Free meal from special menu.
- Chevrolet — GM Military Appreciation special offers (authorization number required).
- Chrysler — $500 Military Bonus Cash (eligible groups; obtain eligibility code).
- Colonial Williamsburg — Free admission for veterans, active duty & families on Veterans Day weekend.
- Country Kitchen Restaurants — Free Country Scramble for veterans/active duty (participating locations).
- Country Music Hall of Fame — Free admission on Nov. 11 for veterans/active duty + up to three guests.
D
- Dell — 10% discount for veterans on Nov. 11 purchases.
- Denny’s — Free Build Your Own Grand Slam (5 a.m.–noon) for veterans/active duty.
- Dodge — $500 Military Bonus Cash (eligible groups; get eligibility code).
- Dollar Car Rental — Military discounts via Veterans Advantage/ID.me (e.g., 5% off; fee waivers; special coupons).
- Dunkin’ — Free donut nationwide; veterans get 10% off donuts and coffee year-round.
E
- Einstein Bros. Bagels — Free medium coffee (hot/iced).
- El Chico Cafe — Veterans/active duty eat free ($20 limit).
- Enterprise Rent-A-Car — 5% off base rates (gov’t leisure); special rates for official travel.
- Express — 5% off in-store purchases.
F
- Foot Locker — 10% off (verify via SheerID; restrictions apply).
- Ford — $500 bonus toward purchase/lease (verify at fordrecognizesu.com).
G
- Gap — 10% off in store with ID.
- GEICO — Up to 15% off.
- General Motors — $500 bonus on select Chevy or $1,000 on select Cadillac.
- Golden Corral — Free dinner (Military Appreciation Night) on Nov. 11 (5 p.m.–close).
- Goodyear Auto Service — 10% off plus free tire/alignment/brake/fuel/fluid checks (schedule ahead).
- Great Clips — Free haircut on Nov. 11 or a coupon for later.
H
- Hard Rock Cafe — Free Legendary Steak Burger on Nov. 11; 15% year-round military discount.
- Harley-Davidson — Up to $1,500 cash on select new models or $250 credit (through Nov. 30).
- Huddle House — Free MVP Breakfast Platter.
I
- IKEA — Free meal for veterans.
J
- J.Crew — 15% off (verify via SheerID or show valid ID).
- Jeep — $500 bonus cash (100% disabled vets and honorably discharged within 1 year).
K
- Krispy Kreme — Free donut and coffee for veterans.
L
- L.L.Bean — Year-round 10% becomes 15% Nov. 1–11.
- Levi’s — 10%–25% off (verify via SheerID).
- Little Caesars — Free Lunch Combo (11 a.m.–2 p.m.; participating locations).
- Logan’s Roadhouse — Free meal from American Roadhouse menu (3–6 p.m.).
M
- Macaroni Grill — Free Mom’s Ricotta Meatballs & Spaghetti.
- Margarita’s Mexican Restaurant — 50% off entrée (dine-in only).
- Mazda — $500 bonus (within 2 years of separation) on purchase/lease.
- Metro Diner — 50% off any meal.
- Microsoft — Up to 10% off select products.
- Mission BBQ — Free sandwich on Veterans Day; live National Anthem at noon.
N
- Nékter Juice Bar — Free 16-oz fresh juice or superfood smoothie.
- Nike — 10% off with military verification.
- Nissan — $500 cash back within 24 months of separation (may combine with incentives).
O
- O’Charley’s — Free meal ($10 value) from Veterans Thank-You Menu (participating locations).
- Olive Garden — Free entrée from special menu (with soup/salad + breadsticks).
- On the Border — Free pick-two combo.
- Orange Leaf Frozen Yogurt — 50% off a cup for veterans/active duty.
- Outback Steakhouse — Free Bloomin’ Onion and Coca-Cola.
P
- Peet’s Coffee — Free drip coffee or tea.
- Perkins — Free Magnificent Seven Breakfast.
- Pie Five Pizza — Free personal pizza (dine-in; participating locations).
- Price Chopper — 11% off one shopping trip on Veterans Day.
- Publix — All veterans and active military personnel will receive a discount of 10% on groceries* on Veterans Day. *This offer excludes prescriptions, alcohol, tobacco, gift cards, lottery tickets, postage stamps, and money services. Valid for in-store purchases only. Customer is responsible for all applicable taxes.
- PUMA — 20% off with verification.
R
- RA Sushi — Free shareable (dine-in).
- Red Lobster — Free appetizer or dessert.
- Reebok — 30% off for veterans and families (verify via ID.me).
- Roy Rogers — Free Uncle Ralph’s brownie with any purchase (participating).
- Russell Speeder’s Car Wash – Free car wash for all veterans and active-duty service members from November 9-11.
S
- Shoney’s — Free all-you-care-to-eat breakfast until 11 a.m.
- Smoothie King — Free 20-oz smoothie (12–3 p.m.).
- Sport Clips — Free haircuts for veterans & active duty at some locations.
- Starbucks — Free tall hot-brewed coffee for veterans, active duty, reservists, and military spouses.
T
- Target — 10% off two purchases.
- TCBY — First 6 oz free.
- Texas Roadhouse — Free meal voucher (11 a.m.–2 p.m.).
U
- Uno’s Pizzeria & Grill — Free entrée/individual pizza with purchase of a second meal (equal/greater value).
V
- Volkswagen — $500 bonus toward a new/leased vehicle.
- Volvo — Incentives vary on purchase/lease of new/used vehicles.
W
- Waters Car Wash – Free car wash for all veterans and active-duty military from November 9-11.
- Wendy’s — Free small breakfast combo (no purchase necessary).
- White Castle — Free breakfast combo or Castle Combo #1–6.
- Wienerschnitzel — Free chili dog + small fries + small Pepsi (ID or uniform).
- Wrangler — 10% off online (verification).
Z
- Ziggi’s Coffee — Free 16-oz drink at all locations.
While no discount can ever match the sacrifices made by America’s veterans and their families, these offers represent one small way for businesses to show gratitude. Whether you’re grabbing a free cup of coffee, a meal, or taking advantage of a year-round discount, these gestures reflect a simple truth: your service matters, and your country remembers.
October highlighted a different kind of service — the kind that takes place quietly, daily, and often without recognition. Warrior caregivers are the spouses, partners, parents, and loved ones who support veterans through transition, trauma, treatment, and the ongoing realities of post-service life. Their role is not secondary; it is central to the veteran experience. This month, we elevated their voices, examined the barriers they face, and spotlighted the care models and peer support networks that are making a difference.
Here’s what you might have missed:
Articles + Blogs
We explored care from every angle, including the GI Bill “kicker” that can increase education benefits, transition challenges unique to women veterans, and how to build peer support circles when formal caregiving support isn’t available. We also honored the lived experience of veteran Don Legun, whose insights helped shape one of our most-read mental wellness pieces of the month.
– Did You Know? The GI Bill “Kicker” Could Boost Your Education Benefits
– The Debt We Owe: Defending Veterans Against a Misguided Narrative
– 17 Ways to Recognize When Your Mental Health Is Shifting
– America’s Hidden Heroes at Home: Caregivers in Veteran and Military Families
– Caring for the Caregivers: Operation Healing Forces Supports Those Who Support Our Heroes
– Our 2026 Veteran Priorities
– Left of Clinical: A New Approach to Veteran Wellness, Parts I, II, and III
– Transition Challenges Unique to Women Veterans
– Building Your Own Support Team: How Veteran-Led Peer Networks Fill the Caregiver Gap
– Veteran Owen Lonsdale’s HBOT Journey
The Lasting Mission Podcast
This month’s episode spotlighted a veteran working to transform the future of care in rural America, building solutions that meet people where they are. Meet Katt Whittenberger from Mountain Valor:
– The Climb Toward Hope: Inside the Mountain Valor Mission – A Hero for Rural Virginia Veterans
Mission Roll Call University (MRCU)
October’s resource focused on career readiness, providing veterans with practical tools to identify available opportunities and connect with employers seeking their unique skills. WATCH: Find Available Career Openings FREE with Oplign.
Veteran Town Hall
Veterans joined CEO Jim Whaley and COO Ray Whitaker to discuss trust in the system, real experiences navigating the VA, and what they need most to thrive in civilian life.
MRC in the Media
Veteran voices resonated nationwide this month as outlets across the country examined the real-world impact of political decisions, shutdown risks, and access to care.
– The Hill || Veteran groups warn Congress against shutdown: ‘Resist the pull of political brinkmanship’
– The Washington Post || I’m a veteran on disability. This reporting hurt me.
– Connecting Vets || Veteran says service dogs serve a purpose
– The Center Square || 91% of U.S. veterans concerned about food assistance amid shutdown
– The National Desk || Veterans worried, confused over government shutdown that’s stretching into second month
Speak Up: Your Voice Matters
Every survey, poll, and comment shared with Mission Roll Call helps guide how we advocate, what policies we elevate, and where we focus our research. Veteran feedback has already shaped national conversations on access to care, mental wellness, and homelessness. Your perspective is the foundation of meaningful change. By sharing your experiences, you help ensure that decision-makers hear directly from those who have served.
– Take the November Community and Belonging Survey
– Explore Open Polls
Looking Ahead: Veterans Day and Beyond
November will be dedicated to honoring the service, sacrifice, and humanity of America’s veterans through their stories, their experiences, and the lasting impact they continue to make every day.
If there is a veteran in your life whose story you carry with you, we invite you to add their name to our 2025 Honor Wall so their service can be honored publicly and preserved. Add a name to the Honor Wall.
Veteran suicide rates have remained stubbornly flat for nearly two decades despite billions invested and countless initiatives. The model we rely on still waits until veterans are already in crisis, and by then, the primary tools left are prescriptions and clinical interventions that treat symptoms but rarely restore purpose or connection. VA’s latest report still reflects thousands of veteran lives lost each year, which is why veterans in our survey delivered a near-unanimous mandate for preventive partnerships. At Mission Roll Call, we believe it is time to test a different path.
In Part One of this series, we examined what veterans lose in transition: the camaraderie, networks, and healthy outlets that once gave them purpose and belonging. In Part Two, we explored what prevention could look like if built left of clinical—fitness, service, mentorship, and creative outlets delivered in ways veterans say they want, and with barriers like cost and awareness removed.
Part Three now asks the hardest question: if veterans overwhelmingly want preventive wellness, who should lead the effort? Our survey results and broader research point to a three-legged stool: the VA providing authority and validation, Congress delivering funding and flexibility, and VSOs and nonprofits supplying the programs veterans already trust. Together, these three legs can finally create the upstream system veterans are asking for.
Part Three: Building Left of Clinical – The Three-Legged Stool of Preventive Wellness
The results of our latest survey leave little room for doubt. When asked if the VA should fund or partner with preventive wellness programs as part of its suicide prevention strategy, 78.5 percent of veterans strongly agreed, and another 17.8 percent agreed. That is as close to a mandate as we will ever see in veteran policy.
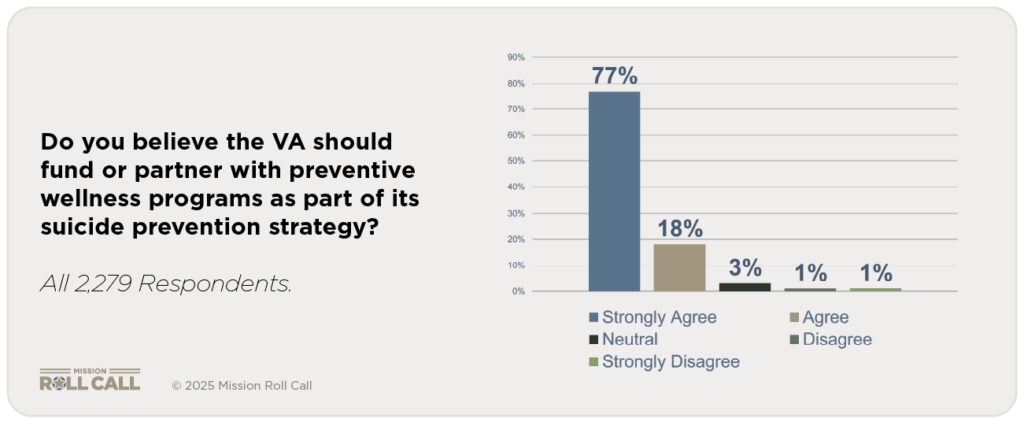
But the VA cannot build this effort alone. Congress cannot simply legislate camaraderie into existence. And while VSOs and nonprofits already deliver strong models of preventive wellness, they cannot scale nationally without support. The solution is a three-legged stool: VA authority, congressional backing, and community partnership. Each leg is essential, and only together can they move the system left of clinical.
The Role of the VA
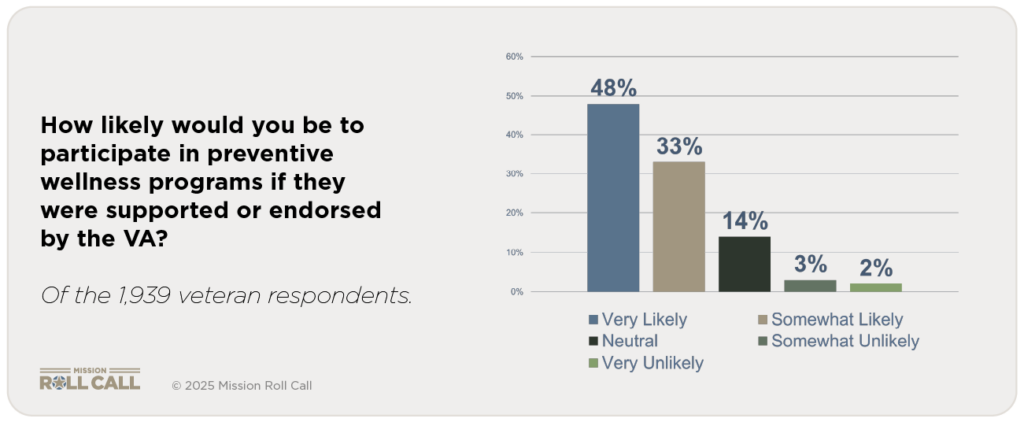
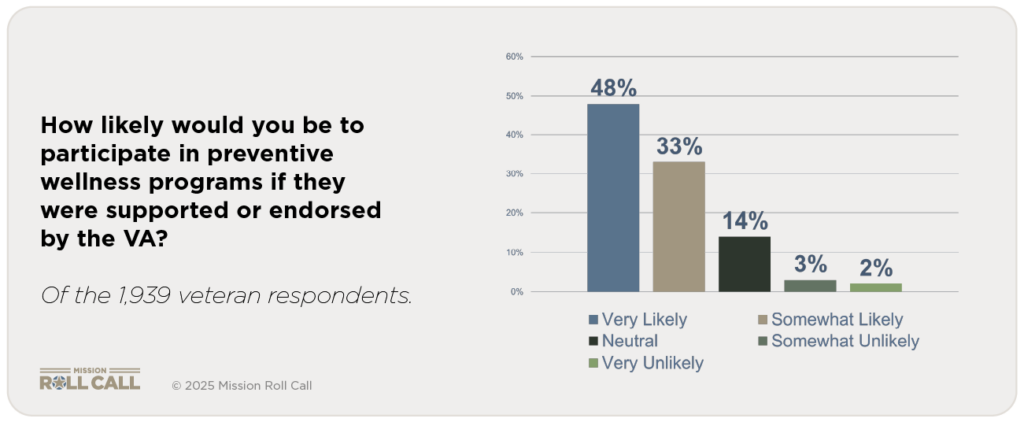
The VA is the anchor. It has the national reach, the trust of veterans, and the authority to set standards. Our survey showed that 48.1 percent of veterans would be “very likely” and another 33.3 percent “somewhat likely” to participate in preventive wellness programs if the VA endorsed them. That endorsement matters. It conveys legitimacy, safety, and continuity of care.
But the VA is not equipped to become a wellness operator. Its infrastructure is built for clinics and claims, rather than rucks, service projects, or peer-led groups. Where it can excel is in convening, validating, and integrating. Through Whole Health programs, Veteran Community Partnerships, and suicide prevention outreach pilots, the VA can create space for preventive wellness to be embedded into transition and care. The VA has some experience with this, though limited in scope, having already piloted community-based social connection models that increased engagement with services.
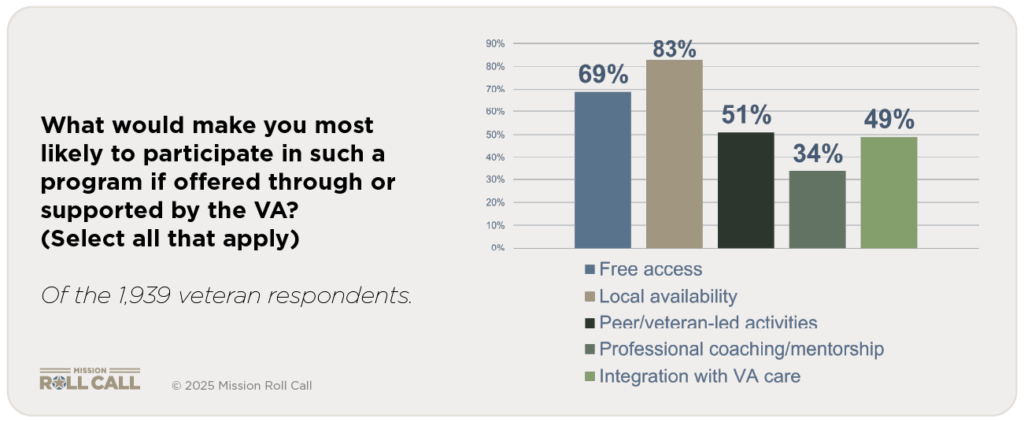
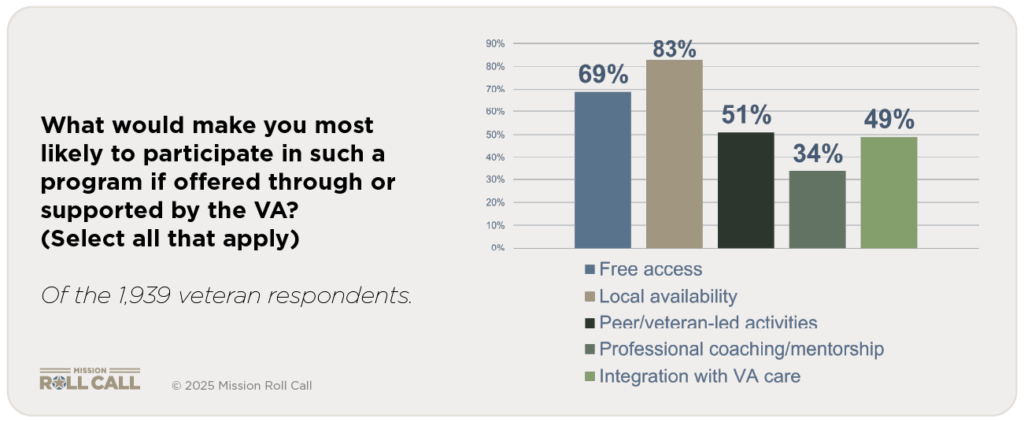
Veterans also told us what would tip the balance: free access, local availability, peer-led activities, and integration with VA systems. Those are levers the VA can pull through grants, co-branding, and referrals that treat preventive wellness as part of the benefit, not a side project.
The Role of Congress
Congress provides the tools. Without targeted legislative support, the VA cannot fund or scale preventive wellness. Congress can:
- Create dedicated funding streams for preventive wellness partnerships with VSOs and nonprofits.
- Expand pilot authorities so the VA can contract directly with non-clinical organizations for fitness, peer support, and community service programs.
- Mandate preventive wellness integration into transition and suicide prevention strategies.
- Provide budget flexibility so dollars can be used for prevention, not only crisis care.
These changes do not require a wholesale rewrite of VA’s mission. They require targeted authorities that enable the VA to meet veterans where they are — before they enter the clinical system. Preventive wellness costs less, produces stronger outcomes, and reduces reliance on polypharmacy and emergency services. Congress can make that possible.
The Role of VSOs and Community Organizations
The third leg of the stool is the nonprofit community. Organizations like Team Red, White & Blue, O2X, GoRuck, The Mission Continues, and Boot Campaign already deliver the kinds of preventive wellness veterans say they want: fitness, service, peer mentorship, creative outlets, and holistic wellness.
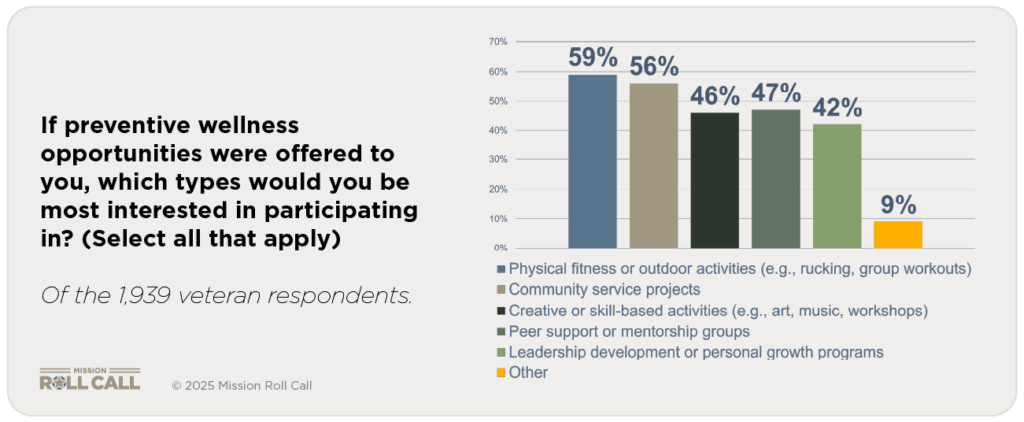
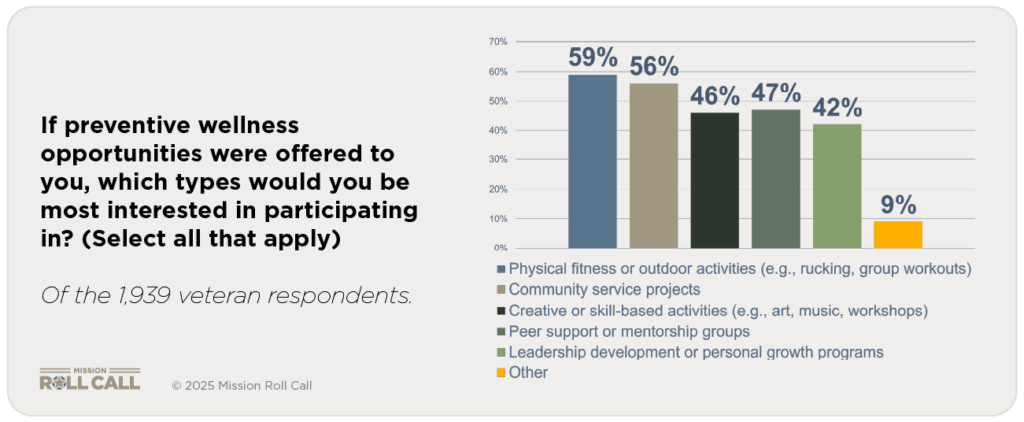
In our survey, when asked which preventive opportunities they would most prefer, veterans pointed to fitness and outdoor activities, community service projects, peer mentorship groups, and creative or skill-based workshops. These are exactly what VSOs and nonprofits already provide.
But nonprofits cannot scale nationally on their own. Their strength is agility, community credibility, and dedication to serving veterans. They know how to design programs veterans trust. What they lack is reach, official backing, and financial stability. That is where VA partnership and congressional support become essential.
The Path Forward
If each leg of the stool plays its part, preventive wellness becomes not only possible but powerful:
- The VA convenes, validates, and integrates preventive wellness into standard services.
- Congress provides the programs, intent, funding, and legal authorities to start small and then scale those efforts nationally.
- VSOs and nonprofits deliver the programs veterans want most, with the credibility and agility only community-based groups can provide.
This is not about a new bureaucracy. Rather, it’s about re-aligning our focus and resources in a way that better meets the needs of veterans. It is about using what already works, aligning it with VA’s reach, and giving it the legislative foundation to last.
Why Left of Clinical Matters
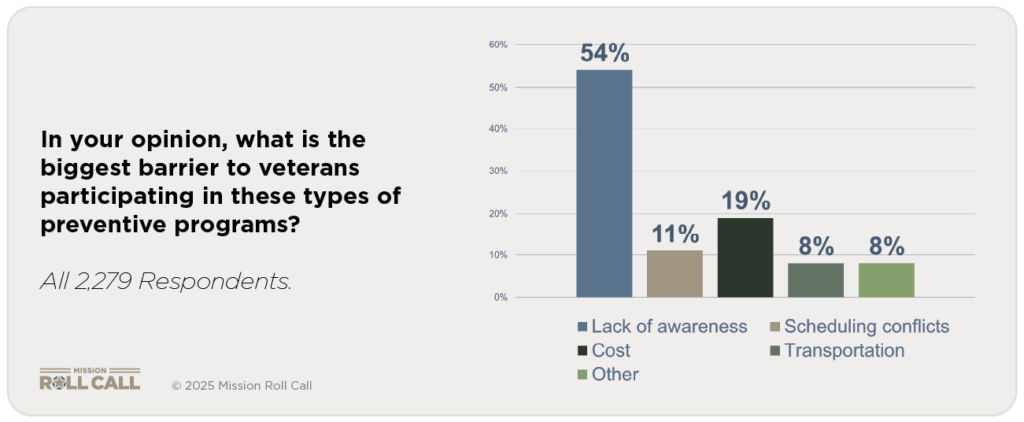
Without this three-legged stool, too many veterans will continue to arrive at the VA only when crisis is at their doorstep. By then, stress has hardened into anxiety, isolation into despair, and the only tools left are medication and clinical intervention. Our survey showed that the biggest barrier today is awareness — 53.7 percent of veterans said they simply don’t know what programs exist.
If the VA, Congress, and VSOs together remove those barriers, preventive wellness can shift the system left of clinical. That is where the real change happens — not just treating crisis, but preventing it by keeping veterans connected, active, and purposeful.
Closing
Veterans want preventive wellness. They know what kinds of programs will help. They are ready to participate if the VA supports them. And they expect their government to act.
The path forward is not VA alone. It is a three-legged stool of VA authority, congressional backing, and nonprofit partnership. Each leg is essential. Together, they can transform preventive wellness from an idea into a national reality — cheaper, more effective, and truer to what veterans say they need.
That is the veteran-led mandate to move left of clinical.
Left of Clinical is a Caregiving Imperative
This three-part series has shown the path veterans are asking us to take. In Part One, we saw the cost of losing camaraderie: isolation, stress, and unhealthy coping. In Part Two, we heard what preventive interventions could look like: fitness, service, mentorship, and creative outlets—accessible and structured to meet veterans where they are. And in Part Three, we mapped the roles of the VA, Congress, and community organizations in building the three-legged stool of preventive wellness.
Veterans are not rejecting clinical care—they are asking us to invest upstream. They want opportunities that keep them strong and connected long before the point of crisis. They want prevention that is cheaper, healthier, and more effective than a prescription.
If policymakers, the VA, and community partners take this mandate seriously, preventive wellness can become more than a concept. It can become a system that keeps veterans engaged, purposeful, and resilient. That is what it means to move Left of Clinical.
When you don’t have a dedicated caregiver, it can feel like you’re going it alone. You may be wondering: who’s going to check in? Who’s going to make sure I’m okay when things get heavy? The good news is, you don’t have to rely solely on a traditional caregiver model. Community is care. For veterans, peer networks and veteran-led groups are proving to be powerful alternatives or complements to formal caregiving.
Why community-based support matters
Veterans often find healing in connection with people who “get it” and have walked the same path. Peer-to-peer programs have been shown to offer real benefits. For example, a study found that veterans identified peer support as offering social support, a sense of purpose, hope, and normalization of symptoms
Another study showed that community-based peer networks helped with reintegration into civilian life. These programs improve social support, enhance coping, and strengthen community connection.
In short, if you don’t have a caregiver, a support circle built from peers, veteran-led groups, or community networks can help fill the gap.
What types of support exist when caregiving isn’t available
- Peer support networks: These are groups where veterans voluntarily support one another by sharing experiences, challenges, and resources. You don’t need to be “in crisis” to join.
- Gallant Few: Assists members of the Ranger community in reintegrating from active duty service to the civilian world. Gallant Few is an Army Ranger-led active duty and veteran military support organization founded in 2010.
- Team Red, White & Blue (Team RWB): Connects veterans through physical activity, leadership development, and community events. Their chapters host weekly runs, yoga, and fitness meetups that help build camaraderie.
- The Warrior’s Journey: Offers online and in-person support groups, mentorship, and spiritual connection for veterans navigating life’s challenges.
- Veterans Recovery Network: Peer-led support groups inside VA medical centers for veterans in recovery from mental health or substance use disorders.
- Veteran-led advocacy and community groups: These groups often combine social connection with a shared mission or volunteer activity. Being part of something bigger than yourself can shift the dynamic from “I need help” to “We’re in this together.”
- The Mission Continues: Empowers veterans to serve through community service projects, creating purpose-driven teams and strong local networks.
- Travis Manion Foundation: Offers leadership and mentorship opportunities for veterans, including school talks and service projects that reinforce identity and community connection.
- Team Rubicon: Serves communities all over the country, from a glacial flood in Alaska to the devastation of Hurricane Helene in the Southeast, from Long Term Recovery operations in Kentucky to wildfire response in California. This veteran-led organization builds belonging through service.
- Local Veteran Service Organizations (VSOs) and community chapters: Groups like the American Legion, Veterans of Foreign Wars (VFW), and others often offer non-clinical support such as weekly gatherings, peer discussions, rides to appointments, or simply regular check-ins.
- Veterans of Foreign Wars (VFW): Beyond benefits claims, many VFW posts host peer check-ins, community meals, and volunteer opportunities.
- American Legion: Offers everything from benefit assistance to youth mentorship programs and local post events like breakfasts and meetings.
- Disabled American Veterans (DAV): Offers transportation to VA medical appointments, local chapter meetings, and peer navigation support for injured veterans.
- Online communities and remote networks: If mobility, geography, or logistics are barriers, virtual groups can help you connect with peers who understand.
- RallyPoint: A social media platform for service members and veterans to ask questions, share stories, and find community.
- Togetherall: A peer support community monitored by clinicians, free to U.S. veterans through the VA, offering a safe online space to talk through struggles anonymously.
- VA’s Peer Support Outreach: The VA offers virtual and in-person peer support services nationwide. You can request to be connected with a trained peer specialist through your local VA medical center.
- RallyPoint: A social media platform for service members and veterans to ask questions, share stories, and find community.
How to build your own informal “care network”
- Acknowledge your needs without shame
Recognizing that you don’t have a caregiver isn’t admitting defeat. It’s being strategic. Consider what you would want: regular check-ins, someone to pick up groceries, a peer to talk to when you’re struggling.
- Reach out rather than isolate
Look for a veteran peer group in your area or online. Ask someone at your local VSO, “Is there a peer-to-peer group for veterans who live alone or need social connection?”
- Create a circle of support
Think smaller than a “caregiver.” Identify two to four people you can count on such as a fellow veteran, a VSO volunteer, a mentor. Ask each one for one specific role. For example: “Will you call me once a week?” or “Will you come over on Saturdays?” This informal network acts like a team instead of putting everything on one person.
- Tap into tech and remote tools
Use apps, online groups, or virtual meet-ups to stay connected. The U.S. Department of Veterans Affairs (VA) reports that trained peer-sponsor networks help transitioning veterans overcome risk factors for isolation and improve outcomes.
- Volunteer or give back
One of the strongest ways to build community is to serve. When you help others, you build relationships, purpose, and reciprocity. That strengthens the network around you.
- Check in on your network regularly
Like any team, your circle needs maintenance. That could mean a quick text, a planned coffee meet-up, or a peer call. Staying connected now can prevent deeper struggles later.
You’re not alone, and you don’t need a traditional caregiver to get support
Not having a caregiver doesn’t mean you’re unsupported. Veterans supporting veterans, and communities embracing shared purpose, offer a powerful alternative. Research shows that peer-led and veteran-led networks improve belonging, reduce isolation, and enhance well-being.
Start today by taking one small action: join a veteran peer group, ask a fellow veteran to be your weekly check-in buddy, or attend a local veteran gathering. Your community is out there. Building your own support team is not only possible — it’s powerful.
Need a place to begin? Explore Mission Roll Call’s Resource Directory to find veteran-led organizations, mental health services, peer networks, and local support programs near you. Whether you’re looking for a group to join or help with navigating your next step, this directory is a great place to start connecting with the care and community you deserve.
Veteran suicide rates have remained stubbornly flat for nearly two decades despite billions invested and countless initiatives. The current model largely waits until veterans are already in crisis, and by then, the tools left are prescriptions and clinical interventions that treat symptoms but rarely restore purpose and connection. At Mission Roll Call, we believe it is time to test a different path.
In Part One of this series, we saw the cost of lost camaraderie. Veterans told us they miss the team, struggle to build new networks, and often lack healthy outlets for stress. Nearly all agreed that structured opportunities for connectedness are essential. Without them, isolation grows, stress compounds, and too many veterans arrive at the VA only when a crisis is at their doorstep.
Part Two asks the next question: what would it look like to act Left of Clinical—to create preventive opportunities for connection, service, and purpose before the prescription pad comes out? Our survey results outline what veterans want, what keeps them from joining today, and what would make participation possible. The answers are clear, practical, and veteran-led.
Part Two: Designing Interventions Left of Clinical
Veterans told us exactly the kinds of interventions they would choose. When asked what preventive wellness opportunities mattered most, the top answers were physical fitness and outdoor activities, community service projects, peer mentorship groups, and creative or skill-based workshops.
These are not exotic solutions. They are the same habits that keep people healthier across all populations: exercise, social connection, meaningful activity, and self-expression. Veterans are pointing to everyday practices that build resilience — only they want them structured, accessible, and veteran-oriented. Independent research from Frontiers in Psychology also confirms that peer- and group-oriented programs have been shown to reduce loneliness and increase purpose and engagement among veterans.
What Keeps Veterans Out
So why aren’t more already engaged in these activities? The biggest barrier, by far, was lack of awareness. More than half of respondents (53.7 percent) said they simply don’t know what programs are available. Cost came next at 18.8 percent, followed by scheduling conflicts (11.3 percent) and transportation (7.5 percent).
This tells us something important: veterans are not rejecting preventive wellness. Most just don’t know it exists or can’t make it fit into their lives. The problem is not demand. The problem is design. This tracks with what we’ve reported at Mission Roll Call about awareness and navigation challenges across VA systems.
What Would Tip the Balance
We also asked what would make veterans more likely to participate. The answers clustered around four practical needs: free access, local availability, peer- or veteran-led activities, and integration with VA care. These directly mirror the barriers: address cost, geography, trust, and legitimacy, and you unlock participation.
This is not about inventing something new, and it points directly to solutions. If we want preventive wellness to be real, we don’t need to invent a new model. We need to remove the obstacles veterans themselves have identified. Independent research from RAND catalogs preventive activities where peer and community strategies complement clinical care, suggesting VA endorsement and integration can multiply impact.
The Power of VA Endorsement
Finally, we asked how likely veterans would be to join preventive wellness programs if the VA supported or endorsed them. Nearly half (48.1 percent) said “very likely,” another 33.3 percent said “somewhat likely,” and only 4.7 percent said unlikely.
That endorsement matters. It signals credibility, safety, and legitimacy. Veterans are telling us they would proactively join preventive opportunities if those opportunities existed and if the VA put its weight behind them.
This is the essence of Left of Clinical. Veterans do not want to wait for crises. They are asking for earlier options that are cheaper, healthier, and more sustainable than endless clinical interventions. Broader research also associates routine physical activity with lower rates of mental-health problems and suicidality, underscoring why fitness-based, peer programs can be smart prevention.
Why This Matters
If half of veterans are already struggling with stress or isolation, and more than 80 percent say they would likely participate in preventive programs if endorsed by the VA, then the opportunity is enormous. We can intercept isolation and despair early. We can substitute connection and purpose for medication and symptom management.
The system has never truly invested in preventive wellness, but the message from veterans is unmistakable: they are ready. In Part Three, we turn to how the VA, Congress, and community organizations can work together to build the three-legged stool that makes preventive wellness real.
Women have served in the U.S. Armed Forces with courage, commitment, and professionalism across generations. Today, women veterans represent one of the fastest-growing populations in the military community. As they transition from military to civilian life, many face distinct challenges in areas such as employment, housing, identity, and health care.
Recognizing and understanding these unique transition challenges is essential for building more inclusive and supportive systems that help all veterans succeed after service.
Employment
Finding meaningful employment after military service is one of the most important steps in a veteran’s transition journey. While many veterans benefit from federal and state-level employment programs, women veterans often face different barriers when reentering the civilian workforce.
Veteran Employment Statistics
In 2024, the overall veteran unemployment rate was 3.0%, with women veterans experiencing a slightly higher rate of 3.5%, compared to 2.9% for male veterans, according to the U.S. Bureau of Labor Statistics (BLS).
Common Employment Challenges
- Translating military experience: Many women serve in roles such as administration, logistics, healthcare, or communications; positions that may be undervalued or misunderstood by civilian employers.
- Workplace bias: Women veterans sometimes face gender-based discrimination or skepticism about their military service, especially in male-dominated industries.
- Caregiving responsibilities: Upon leaving the military, women often resume or continue caregiving duties for children or family members. This can limit access to full-time roles or positions with inflexible hours.
Helpful Resources
Programs like Hire Heroes USA, VA’s Women Veterans Program, and the Department of Labor’s VETS program offer tailored career counseling, resume assistance, and employer outreach for women transitioning to civilian employment.
Housing and Stability
Stable housing is a critical foundation for successful reintegration. While many services exist for homeless veterans, recent data shows that housing insecurity among women veterans is a growing concern.
Housing Statistics
- From 2020 to 2023, homelessness among women veterans rose by 24%, from 3,126 to 3,980.
- Unsheltered homelessness (living in vehicles, on the streets, or in unsafe conditions) increased by 48%, from 1,464 to 2,165 in the same period.
- In FY2024, more than 27,444 women veterans were served through VA homeless programs.
Contributing Factors
- Military Sexual Trauma (MST) and domestic violence histories may impact housing stability.
- Limited access to family-friendly shelters makes it harder for women with children to find transitional housing.
- Underreporting: Women experiencing homelessness are more likely to stay with friends or family than enter shelters, making them less visible to service providers.
Supportive Solutions
Initiatives such as Supportive Services for Veteran Families (SSVF) help provide rent assistance, case management, and long-term housing solutions for women veterans.
Identity and Belonging
A less visible but equally important challenge is the issue of identity and recognition. Many women veterans report feeling unseen or excluded within both military and civilian spheres.
Common Identity Challenges
- Public perception still largely associates military service with men, leading to misconceptions about who qualifies as a veteran.
- Underrepresentation in veteran imagery, leadership, and outreach efforts can cause women to question whether they belong in veteran spaces.
- Women who mention their service may be assumed to be a spouse or family member of a veteran, rather than a veteran themselves.
Rebuilding Identity
Organizations like Women Veterans Alliance, Service Women’s Action Network (SWAN) and Mission Roll Call are working to elevate the voices of women veterans and foster a stronger sense of identity and belonging within the veteran community.
Health Care
Health care remains one of the most critical components of a successful transition. While the Department of Veterans Affairs (VA) continues to expand care options for women, understanding the specific health needs of women veterans is essential to ensuring quality and access.
Key Health Insights
- Military Sexual Trauma (MST) affects about 1 in 3 women veterans using VA services, according to the National Center for PTSD.
- Post-Traumatic Stress Disorder (PTSD) may present differently in women and can go underdiagnosed or misdiagnosed.
- Reproductive health care access is improving, but gaps remain in access to OB/GYN services across some VA locations.
- Suicide risk: Women veterans using VA care are nearly twice as likely to attempt suicide as their male counterparts, per a DAV mental health report.
Resources for Women Veterans
- VA Women’s Health Clinics offer specialized care for reproductive health, mental health, and MST recovery.
- Whole Health programs provide personalized wellness support for veterans.
Strategies and Recommendations
Transitioning from military to civilian life is not a one-size-fits-all experience. For women veterans, it’s essential that transition programs, support systems, and outreach efforts reflect their unique journeys. Listed below are strategies and recommendations we could all advocate for to better support women veterans in the workplace, at home, and in the world.
- Tailor transition programming: Expand content in the Transition Assistance Program (TAP) to address caregiving needs, civilian workforce reentry, and gender-specific challenges.
- Support women-focused housing solutions: Increase access to safe, trauma-informed, and child-friendly transitional housing options for women veterans.
- Strengthen women’s health care access: Ensure all VA facilities have properly staffed women’s clinics, and offer MST-trained providers with same-gender care options when requested.
- Promote visibility and leadership: Highlight women veteran leaders in national campaigns and ensure representation across VA boards and advisory councils.
- Expand outreach and benefit education: Utilize community-based partnerships (e.g., women’s shelters, clinics, colleges) to reach women veterans who may not engage with traditional channels.
Conclusion
At Mission Roll Call, we believe that every veteran’s voice deserves to be heard, and that includes the voices of women who have worn the uniform with pride. As the population of female veterans continues to grow, so too must our commitment to supporting their transition to civilian life, ensuring they have the tools, recognition, and resources they need to thrive. You can help by amplifying women veterans’ stories, hiring those who have served, or supporting organizations dedicated to their success.
By working together — across government, community, and industry — we can build a future where women veterans are not just supported but celebrated.
Veteran suicide rates have remained stubbornly flat for nearly two decades despite billions invested and countless initiatives. VA’s 2024 Annual Report tallied 6,407 veteran suicide deaths in 2022 (17.6 per day), underscoring how little progress the nation has made since 2001. The current model largely waits until veterans are already in crisis, and by then, the tools left are prescriptions and clinical interventions that treat symptoms but rarely restore purpose and connection. We’ve written extensively about the failure of progress in this regard, including our Suicide Prevention page, our survey addressing this topic, and our 2025 Update to our State of Veteran Suicide report. At Mission Roll Call, we believe it is time to test a different path.
In this three-part series, we explore the concept of moving “Left of Clinical”—acting earlier, while veterans are still strong and connected, rather than waiting until isolation and despair drive them to the edge. Our latest national survey of nearly 2,300 veterans and family members makes the case for preventive wellness: interventions that keep veterans engaged, purposeful, and resilient long before they ever need a prescription or diagnosis.
In Part One, we examine what veterans lose in transition and why connection matters. In Part Two, we look at what preventive interventions could actually look like in practice. And in Part Three, we map out how the VA, Congress, and community partners can work together to build a system that finally bends the curve on veteran suicide.
Part One: Veterans Value Preventive Connectedness
At Mission Roll Call, we listen to what veterans are telling us and bring those voices directly into the national conversation. In September 2025, we conducted a survey focused on a question that does not often get asked: what would it look like if the VA, and indeed our entire veteran care system, invested more heavily in preventive wellness programs that keep veterans strong and connected before they ever need medical intervention?
The message is unmistakable. Veterans are asking for a broader array of options that they can tailor to their specific needs, with greater say and influence over those decisions. But here is the harder truth: veteran suicide statistics have remained flat for nearly two decades.
Despite billions of dollars invested, the model we rely on is not moving the needle. We continue to meet veterans at the point of crisis, and too often the only tools available are prescriptions and clinical interventions that treat symptoms without addressing root causes. Preventive wellness offers a new and largely unexplored pathway — one that can help veterans stay connected, purposeful, and healthy long before they ever reach the edge of crisis.
With suicide rates unmoved and trust in current approaches strained, it’s time we begin holding serious discussions about how to achieve these aims.
What “Left of Clinical” Means
The phrase “left of clinical” comes from the same mindset that has guided military training and operations for generations. In military planning, being “left of” something means acting before the moment of crisis. In veteran health, being “left of clinical” means recognizing and addressing the challenges of transition and post-service integration into society long before they result in harmful self-talk or require a diagnosis or prescription.
Today, too many veterans only enter the care system once their struggles have reached a breaking point. Typically, by this point, isolation has taken root, stress has hardened into anxiety, and coping mechanisms have turned unhealthy. Too many veterans respond at that stage with alcohol or medication, or both, sometimes a cocktail of drugs prescribed with the best of intentions, but ultimately are not designed for prevention or long-term wellness and often create long-term dependencies and addiction. A case of the cure being worse than the disease.
Our latest survey gives weight to what many of us already know instinctively: veterans want healthier options long before they get to that point.
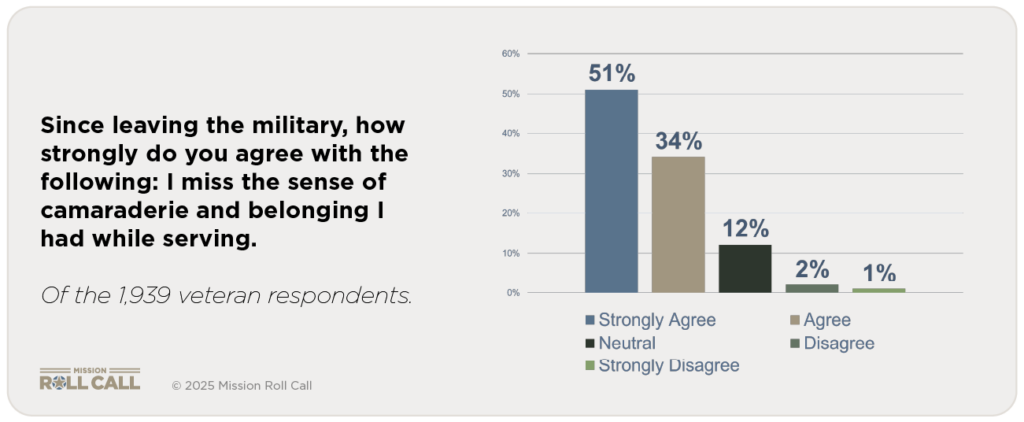
The strongest signal from our September survey is about what veterans value most after leaving the military. Almost 86 percent of respondents said they strongly agree or agree that they miss the sense of camaraderie and belonging they had while serving. Less than 3 percent disagreed. The bond of shared experience is not just a fond memory. It is the anchor that many veterans find missing in civilian life.
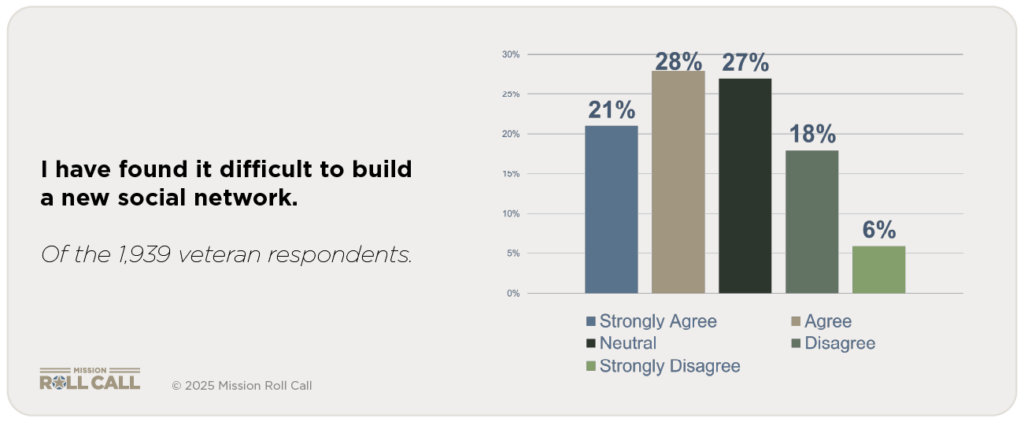
That loss has real consequences. Nearly half (49.5 percent) said they agree or strongly agree that they have found it difficult to build a new social network since leaving the military. Another 27 percent were neutral, meaning only about one in four veterans feels they have successfully rebuilt the same trust and community they once had in uniform. This is where isolation begins, and where stress compounds.
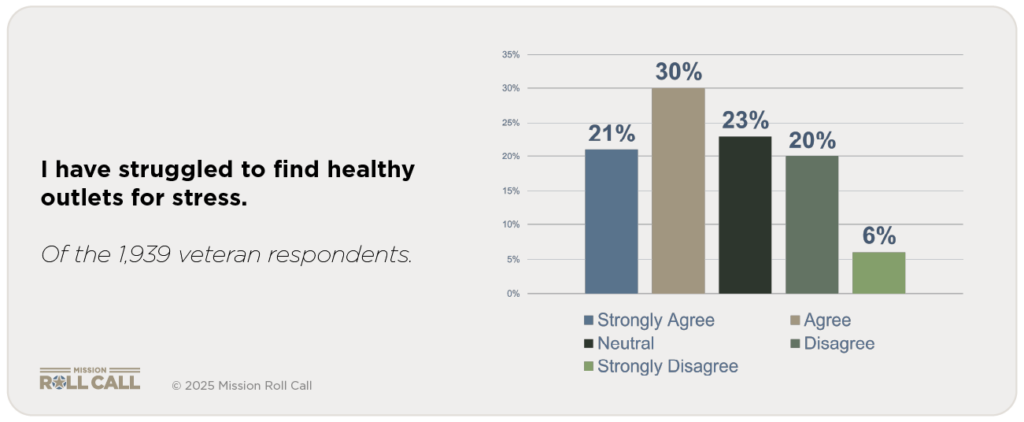
The same pattern appears when veterans talk about coping. Just over 50 percent said they have struggled to find healthy outlets for stress. A quarter were neutral, and only a quarter disagreed. Most veterans live in an environment where the old ways of managing stress—team, mission, shared purpose—are gone, and nothing equally strong has replaced them.
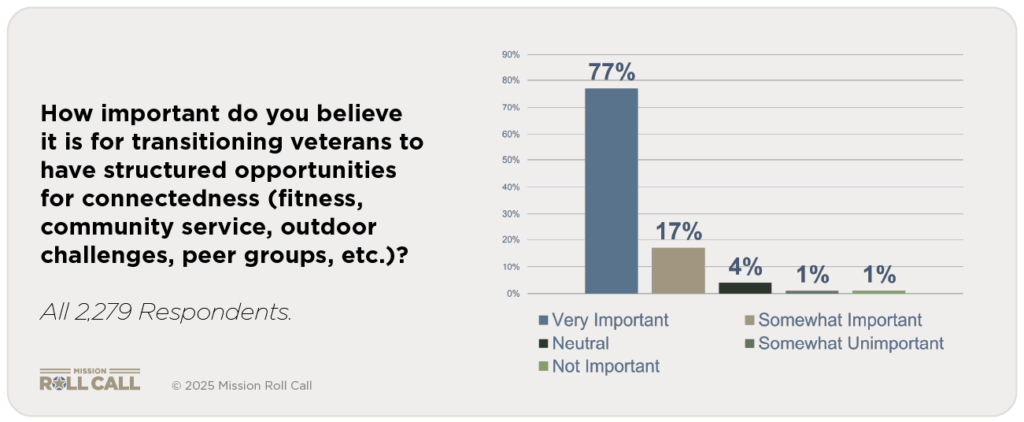
When asked directly, veterans did not hesitate about what they want instead. Over 95 percent said it is very important or somewhat important for transitioning service members to have structured opportunities for connectedness. Less than 1 percent said such opportunities are not important. In other words, nearly every veteran sees connectedness as essential to their well-being.
This matters because of where the absence of connectedness leads. Without community and purpose, isolation grows. Isolation becomes stress. Stress becomes unhealthy coping. And too often, the VA meets veterans for the first time only when they are already in crisis. At that point, the response is often medication—sometimes multiple prescriptions that dull symptoms without addressing the root cause: the loss of belonging.
Veterans are telling us they want something different. They want opportunities to connect, to be part of a team again, to build resilience before they ever need a prescription. They are asking for prevention that sits left of clinical—because they know that is where real strength is rebuilt.
The next question is obvious: what would those preventive wellness opportunities actually look like? In Part Two, we turn to the survey results that show which interventions veterans say they want most, what keeps them out of those programs today, and how the system can remove those barriers.
At Mission Roll Call, everything begins with listening. This year, thousands of veterans, family members, and supporters across the country shared their experiences and perspectives through our annual priorities survey. Together, those voices have shaped our path forward.
Based on what we heard from you, four priorities will guide our work in 2026:
- Access to Quality Healthcare (VA and Non-VA)
- Support for Service-Connected Injuries and Conditions
- Veteran Suicide Prevention
- Housing Access and Homelessness Prevention
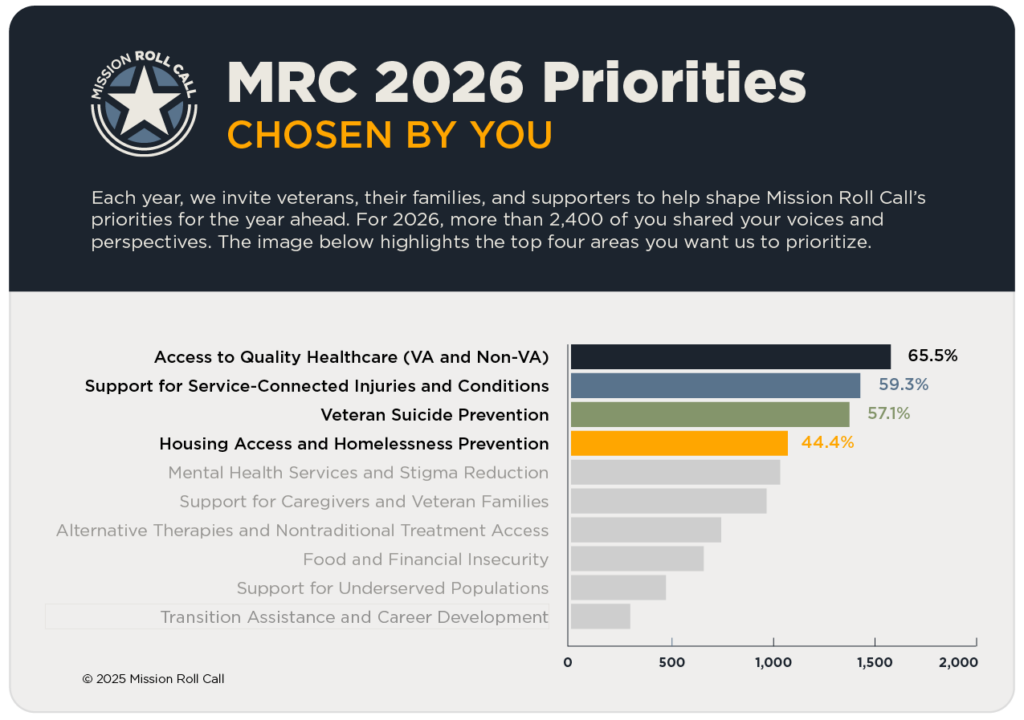
These priorities represent both the challenges veterans and families face and the opportunities we have to create meaningful impact in the year ahead.
When veterans, families, and supporters share their stories with us, they shape national conversations. Veteran feedback directly influences how we advocate, the research we conduct, and the partnerships we build to drive progress. Your voices matter!
Access to Quality Healthcare:
Veterans consistently tell us that timely, high-quality care is one of their most urgent needs. Mission Roll Call is currently conducting research to understand where barriers exist and how to improve care across the system. The findings will be published before the end of 2025 and will help guide our advocacy to make access and outcomes stronger for every veteran.
Support for Service-Connected Injuries and Conditions:
From visible wounds to chronic conditions, many veterans face long-term challenges tied to their service. Mission Roll Call is focused on ensuring they receive the care, benefits, and support they’ve earned. This includes spotlighting policy updates, caregiver perspectives, and programs that promote recovery and independence.
Veteran Suicide Prevention:
Suicide prevention remains a top priority. We are gathering data to better understand risk and resilience among veterans and their families. Through upcoming articles, podcasts, and research, we’ll explore ways to strengthen protective supports and expand preventive approaches to mental wellness.
Housing Access and Homelessness Prevention:
Every veteran deserves a safe place to live. Yet too many remain without stable housing. Mission Roll Call continues to highlight stories, research, and resources that address the root causes of veteran homelessness. To learn more about our efforts in 2025, visit our spotlight page on housing and homelessness.
Working Together for Greater Impact
Mission Roll Call’s work is strengthened by collaboration with Veteran Service Organizations (VSOs) featured in our Veteran Resource Directory. These partnerships help veterans connect to trusted local resources while ensuring that on-the-ground experiences inform our collective efforts.
Throughout 2026, we’ll share updates, research findings, and real stories through articles, blogs, podcasts, and Mission Roll Call University (MRCU). We’ll also report on progress tied to each of these priorities so that the community remains informed and engaged as we move forward.
Why Your Voice Matters
Every story shared and every survey completed moves the mission forward. Veterans and their families help us see where progress is happening and where it’s still needed, guiding how Mission Roll Call educates, informs, engages, and connects.
Because of you, we are turning individual experiences into collective impact. You’re helping build a stronger future for those who have served, and for the generations that will follow.
Thank you for lending your voice to the mission.