Part II, Left of Clinical: A New Approach to Veteran Wellness

Veteran suicide rates have remained stubbornly flat for nearly two decades despite billions invested and countless initiatives. The current model largely waits until veterans are already in crisis, and by then, the tools left are prescriptions and clinical interventions that treat symptoms but rarely restore purpose and connection. At Mission Roll Call, we believe it is time to test a different path.
In Part One of this series, we saw the cost of lost camaraderie. Veterans told us they miss the team, struggle to build new networks, and often lack healthy outlets for stress. Nearly all agreed that structured opportunities for connectedness are essential. Without them, isolation grows, stress compounds, and too many veterans arrive at the VA only when a crisis is at their doorstep.
Part Two asks the next question: what would it look like to act Left of Clinical—to create preventive opportunities for connection, service, and purpose before the prescription pad comes out? Our survey results outline what veterans want, what keeps them from joining today, and what would make participation possible. The answers are clear, practical, and veteran-led.
Part Two: Designing Interventions Left of Clinical
Veterans told us exactly the kinds of interventions they would choose. When asked what preventive wellness opportunities mattered most, the top answers were physical fitness and outdoor activities, community service projects, peer mentorship groups, and creative or skill-based workshops.
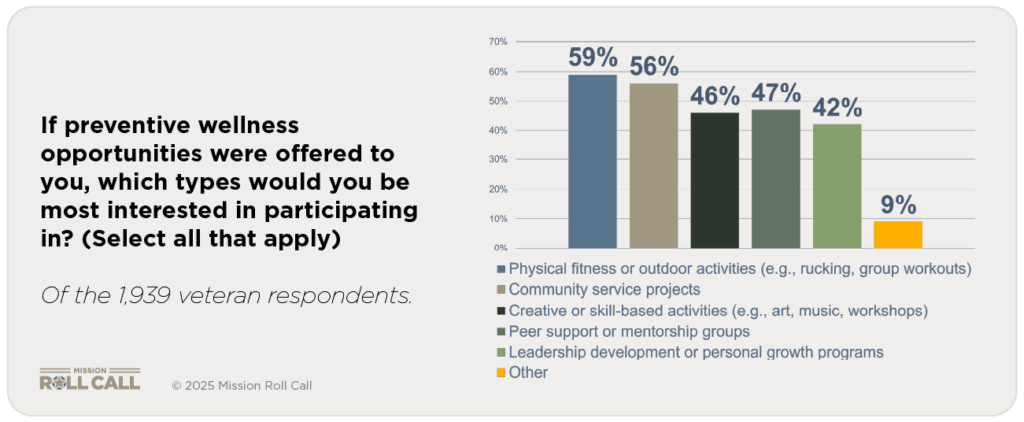
These are not exotic solutions. They are the same habits that keep people healthier across all populations: exercise, social connection, meaningful activity, and self-expression. Veterans are pointing to everyday practices that build resilience — only they want them structured, accessible, and veteran-oriented. Independent research from Frontiers in Psychology also confirms that peer- and group-oriented programs have been shown to reduce loneliness and increase purpose and engagement among veterans.
What Keeps Veterans Out
So why aren’t more already engaged in these activities? The biggest barrier, by far, was lack of awareness. More than half of respondents (53.7 percent) said they simply don’t know what programs are available. Cost came next at 18.8 percent, followed by scheduling conflicts (11.3 percent) and transportation (7.5 percent).
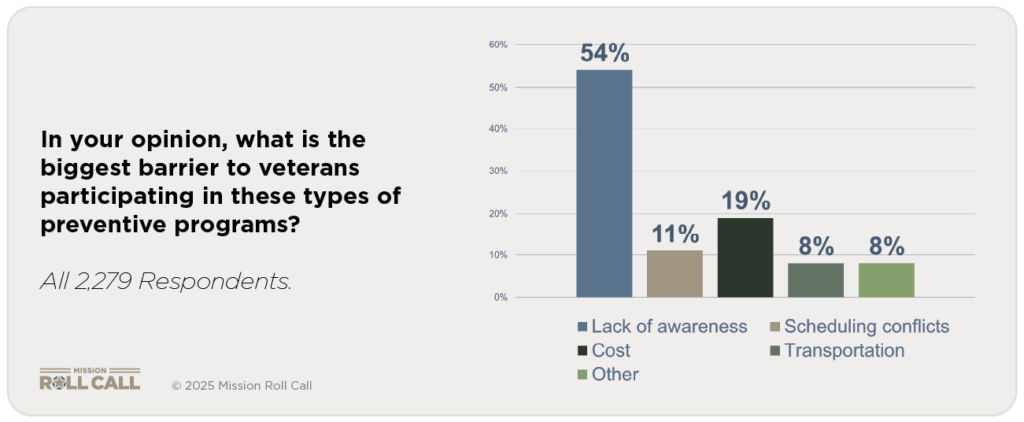
This tells us something important: veterans are not rejecting preventive wellness. Most just don’t know it exists or can’t make it fit into their lives. The problem is not demand. The problem is design. This tracks with what we’ve reported at Mission Roll Call about awareness and navigation challenges across VA systems.
What Would Tip the Balance
We also asked what would make veterans more likely to participate. The answers clustered around four practical needs: free access, local availability, peer- or veteran-led activities, and integration with VA care. These directly mirror the barriers: address cost, geography, trust, and legitimacy, and you unlock participation.
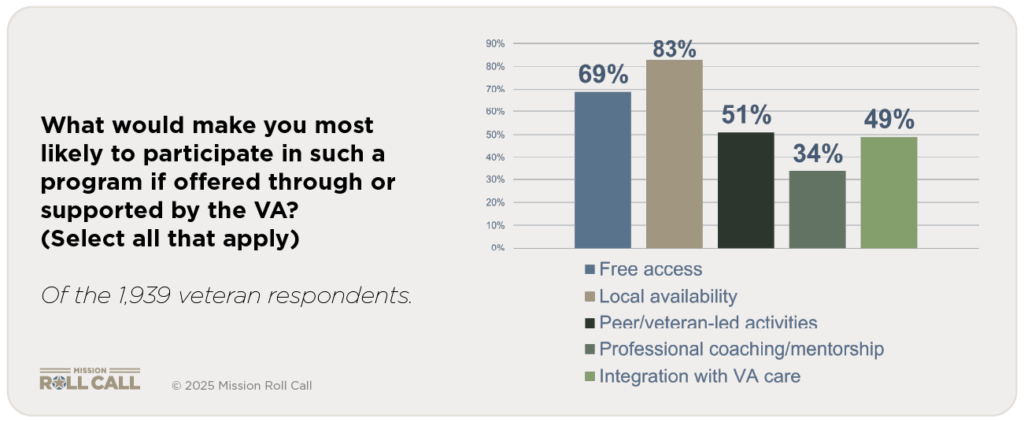
This is not about inventing something new, and it points directly to solutions. If we want preventive wellness to be real, we don’t need to invent a new model. We need to remove the obstacles veterans themselves have identified. Independent research from RAND catalogs preventive activities where peer and community strategies complement clinical care, suggesting VA endorsement and integration can multiply impact.
The Power of VA Endorsement
Finally, we asked how likely veterans would be to join preventive wellness programs if the VA supported or endorsed them. Nearly half (48.1 percent) said “very likely,” another 33.3 percent said “somewhat likely,” and only 4.7 percent said unlikely.
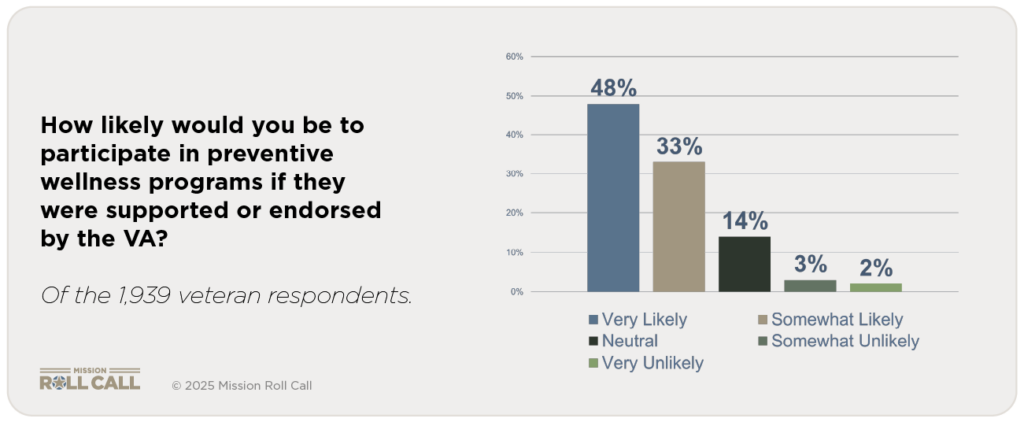
That endorsement matters. It signals credibility, safety, and legitimacy. Veterans are telling us they would proactively join preventive opportunities if those opportunities existed and if the VA put its weight behind them.
This is the essence of Left of Clinical. Veterans do not want to wait for crises. They are asking for earlier options that are cheaper, healthier, and more sustainable than endless clinical interventions. Broader research also associates routine physical activity with lower rates of mental-health problems and suicidality, underscoring why fitness-based, peer programs can be smart prevention.
Why This Matters
If half of veterans are already struggling with stress or isolation, and more than 80 percent say they would likely participate in preventive programs if endorsed by the VA, then the opportunity is enormous. We can intercept isolation and despair early. We can substitute connection and purpose for medication and symptom management.
The system has never truly invested in preventive wellness, but the message from veterans is unmistakable: they are ready. In Part Three, we turn to how the VA, Congress, and community organizations can work together to build the three-legged stool that makes preventive wellness real.