Veterans commit themselves to protecting our nation and preserving our freedoms. Yet after their service, many face unfair obstacles when seeking the healthcare benefits they’ve earned. Limited access to VA facilities, long wait times for care, and a shortage of providers experienced in treating veterans all contribute to the challenges this system is meant to address.
According to a Mission Roll Call survey from August 2022, 86% of American adults believe that Congress has a responsibility to deliver high-quality, timely healthcare for veterans. As military service impacts every community across the country, it’s necessary we find practical solutions to ensure our nation’s former service members receive the care they deserve.
In this piece, we’ll take a closer look at:
- The healthcare benefits currently offered to veterans
- The barriers veterans often face in accessing care.
- The most pressing healthcare issues Congress and the VA should address
- Ways we can better support veterans in getting the medical attention they need
The healthcare benefits currently offered to veterans.
Veterans enrolled in the Department of Veterans Affairs (VA) may qualify for the Basic Medical Benefits Package, which covers a wide range of services, including preventive, primary, and specialty care, as well as diagnostic, inpatient, and outpatient treatments.
In addition to basic coverage, many veterans are eligible for specialized healthcare programs. These include general and specialized mental health services such as treatment for post-traumatic stress (PTS), substance use disorders, and military sexual trauma; available through outpatient and inpatient care.
Eligible veterans may also access outpatient dental services, which can include preventive care, diagnostics, surgeries, and restorative procedures.
The Veterans Health Administration (VHA), a division of the VA led by the Under Secretary for Health, is responsible for delivering healthcare to veterans. As the largest healthcare system in the United States, the VHA provides care to over 9.1 million enrolled veterans across 1,380 facilities, including 170 VA medical centers and 1,193 outpatient clinics.
Despite the breadth of services, many veterans, particularly those who are retiring or transitioning out of service, find the system confusing and difficult to navigate. The 9 million veterans currently enrolled in the VHA represent only about half of the total veteran population. As veterans experience higher rates of PTS due to the demands of military service, this leads to mental health challenges and quality of life. Furthermore, the RAND Center for Military Health Policy Research reports fewer than half of veterans who need mental health care receive it, and among those who do, less than one-third get evidence-based treatment.
To address these systemic shortcomings, lawmakers must expand mental health services, improve access to providers in rural areas, reduce appointment wait times, and expand community-based care options.
The barriers veterans often face in accessing care.
When trying to access VA healthcare, some of the barriers veterans face are limited awareness of available benefits, navigating complex systems, inadequate mental health resources, long wait times, and poor access to VA facilities, especially in rural areas.
The VA reports 18 million veterans in the United States as of 2025. Yet just over 9 million are enrolled in the VA healthcare system. As nearly half of all veterans are not connected to VA services, one contributing factor is the difficulties of transitioning from military to civilian life.
As veterans often face an overwhelming combination of tasks when transitioning to civilian life, the VA’s Transition Assistance Program (TAP) provides a comprehensive framework for supporting service members as they transition back into civilian life. However, many veterans have expressed that TAP doesn’t go far enough and a need for more targeted assistance in adapting to new work environments, finding affordable housing, and accessing both physical and mental healthcare.
These concerns are echoed in the Military Family Advisory Network’s 2023 report on family support services. In a survey of 10,149 military and veteran families, participants identified access to VA healthcare as one of their top concerns. Common issues included trouble booking appointments, delays in receiving care, negative experiences with providers, and dissatisfaction with the quality of services. Notably, the shortage of available appointments was a recurring and urgent concern, particularly in both general and mental health care.
The mental health crisis among veterans is especially alarming given that they are significantly more likely to die by suicide than nonveterans. According to America’s Warrior Partnership’s 2022 interim report, an estimated 40 to 44 former service members die each day from suicide or self-inflicted injuries.
While PTS and other mental health conditions are critical factors, they are only part of the picture. Research has identified additional contributors such as military culture, moral injury, and sexual trauma. Without adequate mental health support, many veterans in crisis may resort to harmful coping mechanisms, including self-harm.
Findings from the Wounded Warrior Project’s 2025 survey of post-9/11 wounded veterans highlight the severity of the issue:
76% reported experiencing symptoms of PTS
50% had moderate to severe symptoms of multiple mental health conditions, including depression and anxiety
28% had experienced suicidal thoughts within the past year
These statistics point to a clear and urgent need to expand and strengthen VA mental health services. In a February 2023 Mission Roll Call poll of 7,200 veterans, 94% said that former service members facing mental health challenges should be able to access care from the provider of their choice, even if they are outside the VA system.
Despite the need, many veterans still struggle to receive proper care. Other barriers to accessing timely and effective healthcare remain persistent. Long wait times, for example, have plagued the VA system for years. A 2014 audit revealed that more than 1,700 patients were placed on secret waitlists at the Phoenix VA, with some reportedly dying before being seen. Though reforms have been introduced since, an April 2022 audit by the VA Inspector General found ongoing issues with how wait times are reported, often masking the actual delays veterans face.
Part of the problem lies in how appointment wait times are calculated. Previously, wait time began from the “request date” provided by either the provider or the patient. But under the current Access to Care system, launched in 2017, wait times are measured from the “create date”, the day a scheduler books the appointment.
For example, in one audit, a veteran referred to a cardiologist had their appointment scheduled a month later. Due to the way VA calculates wait times, the system recorded a 43-day wait instead of the actual 66-day delay.
Furthermore, geographic disparities further complicate access. Nearly 25% of U.S. service members return to rural areas after serving, and today, an estimated 2.7 million veterans live in these communities. According to a February 2023 Government Accountability Office (GAO) report, VHA officials confirmed that rural veterans face distinct challenges due to staffing shortages and transportation difficulties.
The GAO also analyzed 2021 data and found that only 21% of rural veterans used VA outpatient services, compared to 79% of urban veterans, highlighting a stark imbalance in access to care.
The most pressing healthcare issues Congress and the VA should address
To honor the service of our veterans, Congress and the VA have introduced several bills in the first months of 2025 to better serve veterans and provide for post-traumatic growth.
- The MISSION Act,
- Originally enacted in 2018, the law was designed to improve access, transparency, and quality within the VA healthcare system. In 2025, Congress introduced an updated version of the MISSION Act that includes stronger oversight mechanisms, increased funding for mental health programs, and improved care coordination for veterans using both VA and non-VA providers. It also focuses resources on underserved rural areas and reinforcing recruitment efforts for medical professionals trained in veteran care.
- The passage of the Elizabeth Dole 21st Century Veterans Healthcare and Benefits Improvement Act in early 2025 expanded home and community-based care opportunities for veterans, including provisions for caregiver wellness and support.
- Veterans Mental Health Crisis Referral Enhancement Act
- Introduced in February 2025, this bill would increase mental health care accessibility by launching a pilot program in which the VA must provide veterans experiencing mental health emergencies with referrals to approved non-VA mental health care providers.
- Building Resources and Access for Veterans’ Mental Health Engagement (BRAVE) Act
- Introduced in April 2025, this bill looks to strengthen the mental health workforce, infrastructure, and services provided by the VA by taking actions such as extending the Fox Gordon Suicide Prevention Grant Program and improving veteran outreach efforts by vet centers.
- TBI and PTSD Treatment Act
- Introduced in January 2025, this bill aims to provide hyperbaric oxygen therapy to veterans with TBI (traumatic brain injury) or PTSD through the Veterans Community Care Program.
- The VA expanded benefits eligibility to over 3.5 million veterans after the PACT Act was passed in August 2022. The VA also launched a mobile application called VA: Health and Benefits, meant to centralize veterans’ health and benefits information and streamline navigation of VA services.
These legislative efforts reflect a growing recognition that supporting veterans extends beyond meeting basic medical needs to also fostering long-term wellness and opportunities after service. As Congress and the VA continue to make progress, their continued focus must remain on removing barriers, expanding access, and prioritizing mental, emotional, and physical health to ensure every veteran has a path to healing and growth.
Ways we can better support veterans in getting the medical attention they need.
If looking to support the veterans in your life, one of the most impactful things you can do is help them access accurate information about VA healthcare benefits and available providers. You can also advocate on a broader scale by contacting your congressional representatives via email, phone, or letter, urging them to prioritize access to veteran healthcare and reform.
Veterans represent a vital and honored segment of our nation. Their service and sacrifice have helped shape the freedoms we enjoy today, and in return, they deserve efficient, accessible healthcare and robust mental health support.
At Mission Roll Call (MRC), we are committed to expanding healthcare access for veterans nationwide. Through a bipartisan approach, we work to ensure that policymakers in Washington are actively considering the day-to-day realities veterans face.
We also strive to keep our community informed and connected to resources. MRC has partnered with organizations like America’s Warrior Partnership, Patriot Paws, Panhandle Warrior Partnership, Black Ops Rescue, Sierra Delta, Higher Ground, Camp Southern Ground, and Boulder Crest Foundation to expand support networks and access to care.
Through ongoing outreach, polling, and media engagement, MRC continues to advocate for meaningful solutions. By raising awareness and speaking out in our communities, we can help drive the changes our veterans deserve.
Introduction
For decades, the issue of veteran suicide has hovered just beneath the surface of national discourse—tragic, persistent, and alarmingly consistent. Each year, thousands of former service members die by suicide, and the message is tragically clear: we are losing too many of our nation’s heroes after they come home.
Those thousands of lives are not just numbers. They are the men and women who served our nation and who, too often, are left to struggle in silence. These statistics are not new. They echo the same refrain we’ve heard for years. But even slight shifts in data and emerging trends remind us that this crisis is dynamic, and that every year brings fresh opportunities—and obligations—to act.
In this updated report, Mission Roll Call outlines what has changed, what progress has been made, and where we still fall short. With new legislation, shifting budget priorities, and a continued national conversation about mental health, there is hope. But hope alone will not solve the problem. It takes policy, persistence, and the collective will of communities across the nation.
What has changed?
While many suicide-related statistics remain troublingly static, new data and federal actions present important developments.
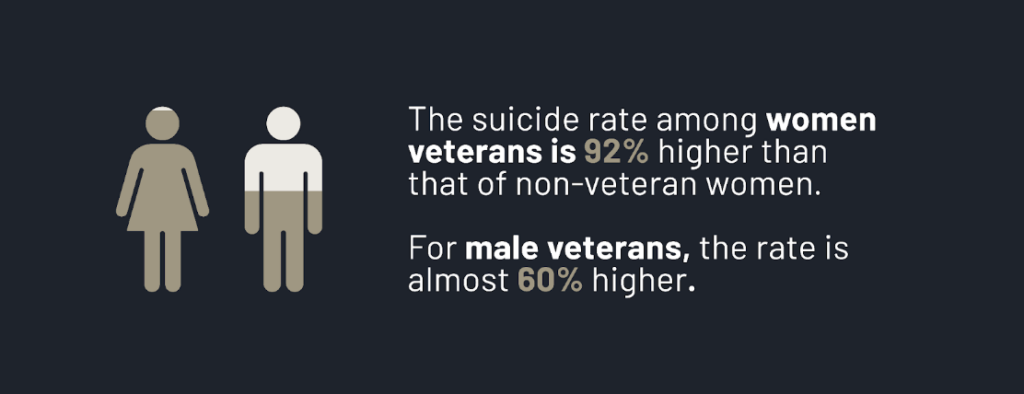
For instance, mental health disparities between veterans and civilians continue to widen. The suicide rate among women veterans is 92% higher than that of non-veteran women. For male veterans, the rate is almost 60% higher. These gaps demand continued focus.
Also worth noting is a growing sense of moral injury and disillusionment among some post-9/11 veterans. Recent data found that 73% of veterans polled felt the U.S. withdrawal from Afghanistan negatively impacted the way they view America’s legacy in the Global War on Terror – a 3% increase from last year.
On a positive note, the annual VA budget has dramatically increased. Over the past decade, the proposed VA budget has increased by 125.3%, reaching $369.3 billion. The VA budget is now more than six times its 2001 budget of $45 billion. This funding is critical and will go toward much-needed health care, benefits, housing and insurance for veterans. Additionally, in May 2025, the Trump administration highlighted the need to honor veterans, stating that the federal government “should treat veterans like the heroes they are.” As part of this commitment, the administration signed an executive order to combat veteran homelessness by establishing the National Center for Warrior Independence, aiming to house 6,000 veterans by 2028.
This kind of momentum is crucial. But funding alone is not enough if it doesn’t translate into real, effective support on the ground.
Veteran suicide by the numbers
According to the VA’s most recent National Veteran Suicide Prevention Annual Report (2024), an average of 17.6 veterans die by suicide every single day. Although this figure is widely accepted, the real number may be even higher.
An Operation Deep Dive report by America’s Warrior Partnership (AWP) suggests that veteran suicides are significantly underreported. AWP suggests that as many as 24 veterans die by suicide per day, with an additional 20 dying by “self-injury mortality,” often overdoses. This totals to a staggering 44 veterans who die by suicide per day, about 2.4 times more than the VA’s estimate.
Mission Roll Call acknowledges the VA’s cautious approach in classifying overdoses as suicides. But the discrepancy between these two reports highlights a deeper issue: we need better data, better definitions, and more transparent reporting. Without accurate data, prevention strategies will always fall short.
Even more urgently, the first two years after leaving active duty remain a high-risk period. Veterans early in their transition often face isolation, unemployment, housing instability, and confusion navigating care. Research from the American Enterprise Institute highlights that the most effective point of intervention is during these first two years, when veterans are actively transitioning, and that critical interventions such as mentoring and job preparation can significantly ease this process. The Departments of Defense and Veterans Affairs must work together more seamlessly to ensure no service member falls through the cracks during this vulnerable time.
Legislative wins: The Elizabeth Dole Act
One major shift in the effort to end veteran suicide comes with the passage of the Elizabeth Dole 21st Century Veterans Healthcare and Benefits Improvement Act. Passed in late 2024, the act is a major legislative win and is the most significant expansion of VA services since the PACT Act. Building on the framework of the PACT Act, which addressed toxic exposure-related healthcare, the Elizabeth Dole Act takes a more holistic approach—expanding VA services to support not just veterans, but also their families and caregivers.
The Elizabeth Dole Act directly benefits veterans by streamlining the disability claims process and expanding job training and employment programs to help them transition to the civilian workforce. It will also increase access to mental health services and support homelessness prevention efforts by identifying at-risk veterans and providing them with funding for job training and substance abuse treatment. The act will also address homelessness by allowing the VA to supply veterans with necessities like food, bedding, hygiene products, and transportation to medical appointments.
On top of serving veterans, the act also serves the 7.8 million military and veteran caregivers – often spouses, parents and dependents – who sacrifice their time and even their personal lives to care for their loved ones. The legislation supports caregivers by expanding caregiver support programs and access to at-home and community-based services across VA medical centers. However, one of the most helpful changes for caregivers is the mental health care grant program, which will fully fund the cost of nursing home care for veterans seeking noninstitutional care alternatives. This could provide eligible veterans and their families thousands of additional dollars per month, easing burdens for aging and disabled veterans and their caregivers.
What work still needs to be done?
Despite this progress, there is more to do. For instance, post-traumatic stress (PTS) remains a leading factor in veteran suicide. Among veterans who served in Iraq or Afghanistan, 15% experience PTS symptoms in any given year, and about a third are estimated to face PTS at some point in their lifetime. Due to its prevalence, PTS is now known as the “signature wound” of the Global War on Terror. Difficult-to-navigate health care only exacerbates this issue, and is unfortunately common: Nearly 45% of veterans experience delays or postponement related to health care services at VA facilities. For instance, the Washington, D.C. VA medical center, which services over 125,000 veterans, has a wait time of 13 days for primary care — but for new patients this time jumps to 43 days. Mental health care is even worse, with 19 day wait time for existing patients, and 53 day wait for new patients, who may be experiencing true issues.
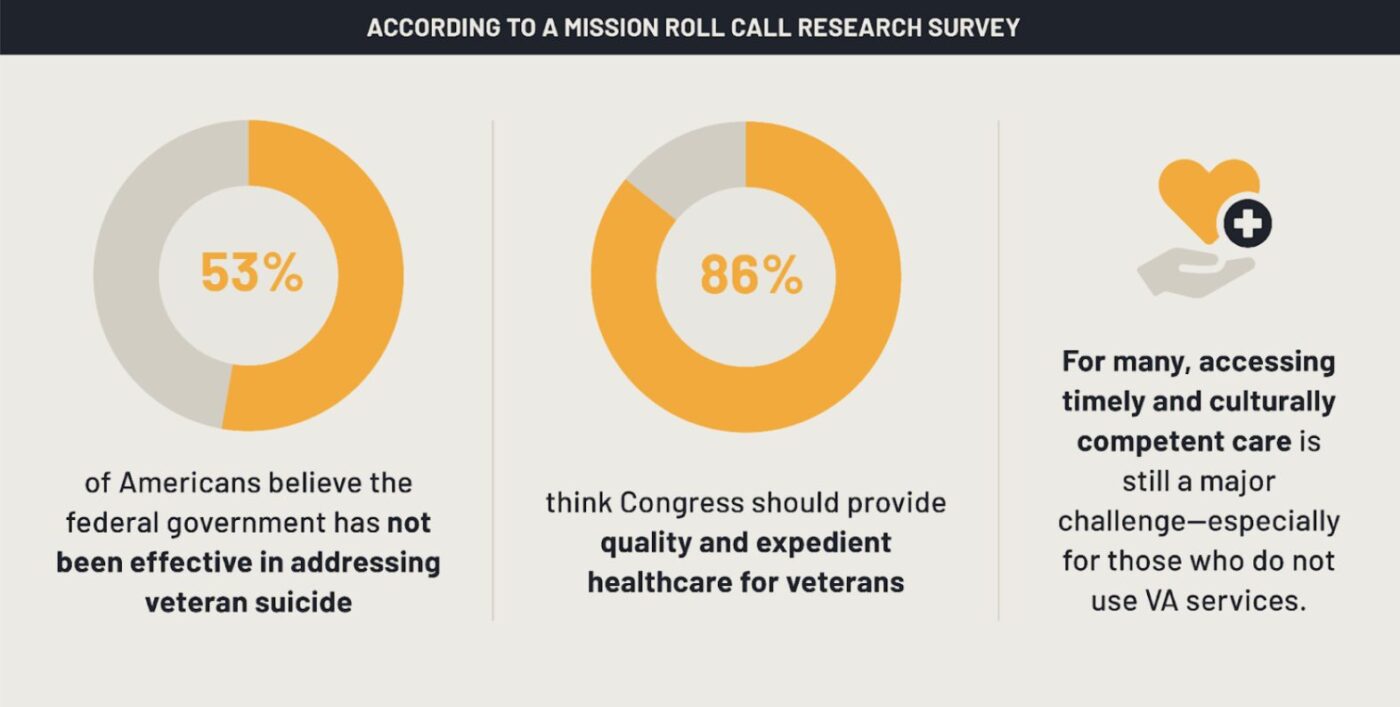
According to a Mission Roll Call research survey, 53% of Americans believe the federal government has not been effective in addressing veteran suicide, and 86% think Congress should provide quality and expedient healthcare for veterans. For many, accessing timely and culturally competent care is still a major challenge—especially for those who do not use VA services.
In our 2024 State of Veteran Suicide report, we highlighted several systemic challenges: inconsistent access to care, gaps in transition assistance, and a dangerous stigma around asking for help. Unfortunately, these issues remain largely unresolved. Legislation like the Elizabeth Dole Act is a significant step toward ensuring veterans and their families receive all the support they need, but it must be part of a sustained, broader commitment to veteran suicide prevention.
How can we help?
Since 2001, the U.S. has lost more than 120,000 veterans to suicide—more than the total American combat deaths in every war since Vietnam combined. This is not a crisis we can address passively. It requires the full force of government, community, and individual action. Since 2001, an alarming 6,000 to 6,700 veterans have died by suicide each year.
Here are some of the ways we can all help:
- Increase mental health access. This means more providers, shorter wait times, and non-pharmacological options like Boulder Crest’s posttraumatic growth program.
- Combat stigma. Many veterans still view asking for help as a weakness. We must continue normalizing mental health conversations in the military community—and beyond.
- Strengthen transition support. Leaving military service should not mean entering a void. Every veteran needs a roadmap—and a community—during their first years of civilian life.
- Support local organizations. Nonprofits like Mission 22, Boulder Crest, and America’s Warrior Partnership are on the frontlines of suicide prevention.
- Re-think suicide prevention models. Suicide rates have remained unchanged after decades of war, and in many ways, mental health and suicide prevention methods have also stagnated. We must rethink this model and aggressively incorporate promising new treatment models including peer-to-peer mental health and preventative wellness activities like HBOT, Team RWB, and O2X.
We must also empower family members and loved ones to recognize warning signs and encourage treatment. Community engagement—not just government programs—will be the true turning point in ending this crisis.
Conclusion
Veteran suicide is a national emergency—one that demands urgency, transparency, and a unified response. While increased funding, new legislation, and executive commitments show promise, the core challenge remains unchanged: far too many of our nation’s veterans are dying by suicide, and we have yet to shift the trend meaningfully.
Mission Roll Call will continue to advocate for smarter policies, more effective programs, and a deeper national commitment to those who served. Together—with clarity, compassion, and sustained pressure—we can build a system that honors their service not just in word, but in action.
Since the 9/11 terrorist attacks, more than 3.3 million veterans have served in uniform, with less than 1% of the American population serving during any given year. 200,000 service members transition to civilian life each year, but less than 50% of veterans are enrolled in VA healthcare, making it imperative for the Department of Veterans Affairs (VA) to change their outreach strategy so veterans receive the health care and benefits they earned and deserve.
An estimated 41% of veterans are in need of mental health care programs every year. Mental health and suicide among veterans is a complicated problem to tackle. There’s no one cause and no one solution. But we do know we need to be more proactive. VA reports have found that veterans are most vulnerable in the first three months following separation from military service, although suicide risk “remains elevated for years after the transition.”
Legislation like the Hannon Act (2020) was an important step toward supporting veterans’ mental health care needs, but there is still much to be done.
In this article, we will discuss:
- What are the most common mental health challenges for veterans?
- What is the Commander John Scott Hannon Veterans Mental Health Care Improvement Act (Hannon Act)?
- What is the Staff Sergeant Parker Gordon Fox Suicide Prevention Grant program (a.k.a. Fox Grants)?
- Why is the suicide rate higher among veterans?
- How can we support veterans’ mental health?
What are the most common mental health challenges for veterans in 2024?
The most common mental health challenges for veterans are post-traumatic stress (PTS), traumatic brain injury (TBI), depression, anxiety and substance abuse.
Mental health issues can affect every aspect of a veteran’s life. In a 2022 study, 38% of veterans had a code on their medical record for a common mental health disorder. This number does not include undiagnosed mental health conditions, which means the actual number is likely much higher.
Post-traumatic stress (PTS) is a condition that can develop after witnessing or experiencing a tragic or traumatizing event. More than a million veterans have been deployed to combat zones since 2001, and according to the U.S. Department of Veteran Affairs, 15% of military personnel who served in Iraq or Afghanistan experience post-traumatic stress each year. 23% of veterans using VA care have had PTS at some point in their lives.
A JAMA Psychiatry study found that the rate of post-traumatic stress is up to 15 times higher among veterans than among civilians. Symptoms include flashbacks, nightmares, avoidance and physical symptoms.
Traumatic brain injury (TBI) can also impact mental health among veterans.
Military service members and veterans can experience brain injury from explosions during combat or training exercises. The Defense and Veterans Brain Injury Center (DVBIC) reported more than 400,000 TBIs among U.S. service members who served since 2000, and more than 185,000 veterans who use the VA for their health care have been diagnosed with at least one TBI.
TBI can cause conditions like headaches, irritability, sleep disorders and depression and can play a major role in veterans’ mental health.
Veterans also struggle with anxiety and depression.
Veterans are five times more likely to experience major depression than civilians, and 3 in 10 veterans with TBI have depression. This can manifest in substance abuse disorders, including alcohol abuse. Some veterans use alcohol and drugs to self-medicate after trauma. Ten percent of Iraq and Afghanistan veterans treated by the VA have a problem with drugs or alcohol.
What is the Hannon Act, and how does it impact veterans’ mental health?
The Commander John Scott Hannon Veterans Mental Health Care Improvement (Hannon) Act expands mental health care options for veterans through grant programs and and suicide prevention programs, especially in underserved communities.
The Hannon Act was inspired by the service of Commander John Scott Hannon, who retired after a decorated 23-year career with the Navy SEALs. Commander Hannon died by suicide on February 25, 2018, at the age of 46.
The Hannon Act includes:
- Grants that will expand community-based suicide prevention and telehealth services to reach veterans in remote areas.
- Funding for mental health research to identify, improve, and expand treatment protocols.
- A pilot program exploring alternative mental health treatments for veterans, including animal therapy, art therapy, sports therapy, yoga, meditation, acupuncture and chiropractic care.
- The Staff Sergeant Parker Gordon Fox Suicide Prevention Grant Program, which dedicates resources toward community-based suicide prevention efforts for veterans and their families.
Congress passed the Hannon Act on August 5, 2020, and President Donald Trump signed the Hannon Act into law on October 17, 2020.
But there is still more work to be done. More than two years after the Hannon Act was passed, for example, the veteran suicide hotline reached its highest-ever number of calls received. This could be because more veterans are comfortable reaching out for help. More likely, however, is that crisis cases are simply increasing.
It’s not enough to simply set money aside. The VA must take an active role in getting funding for mental health programs to the right people, making sure it is accessible to the nonprofits, businesses and community organizations that are on the front lines of veteran care.
What is the Fox Grant and how does it impact veterans’ mental health?
The Staff Sergeant Parker Gordon Fox Suicide Prevention Grant Program, or Fox Grant, is a part of the Hannon Act. The Fox Grant allocates funding for “on the ground” community organizations that offer traditional and nontraditional suicide prevention to veterans and their families.
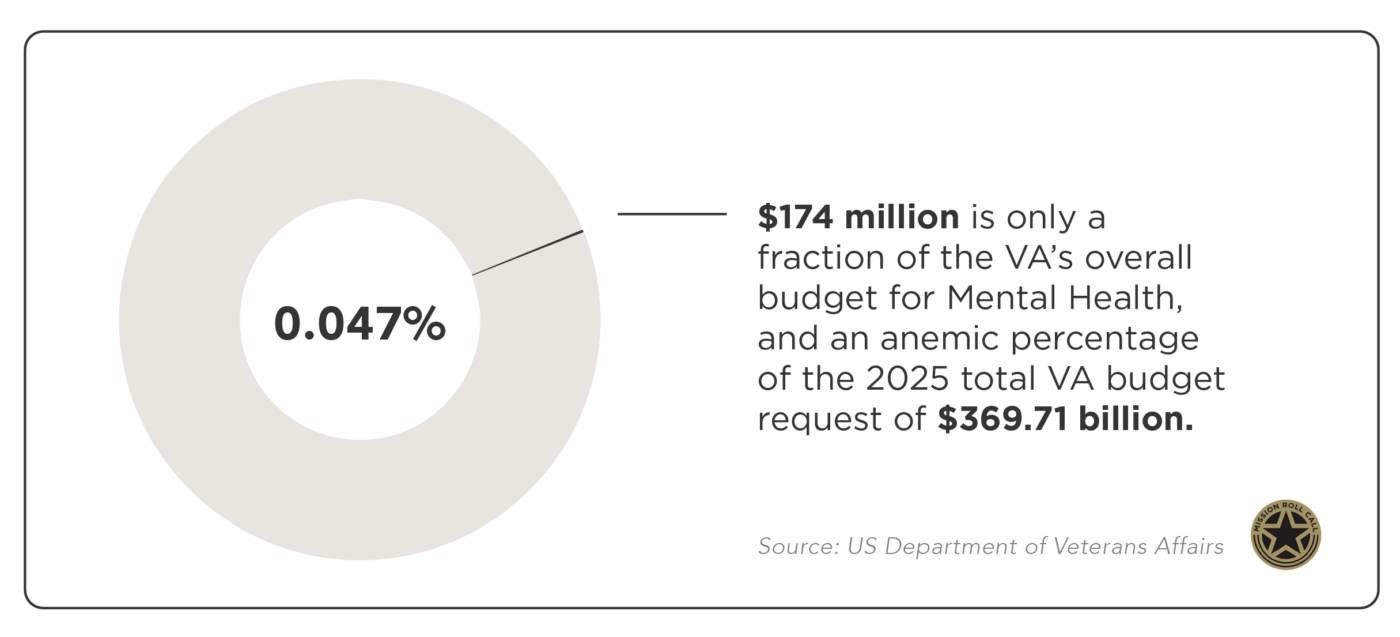
The Fox Grant provided a total of $174 million in resources over three years to veteran-supported community organizations nationwide. The first awards were issued in September 2022, and its final year of funding is FY25.
The Fox Grants have been very successful, but MRC advocates for the FOX Grant program to be permanently authorized beyond FY25 with a more robust appropriation.
Some regulatory changes are needed if the program gets permanently authorized. First, there should be a longer application window for grants. Second, reporting requirements should be tailored to ensure that smaller, valuable organizations can keep up with the workload required by VA.
Additionally, $174 million is only a fraction of the VA’s overall budget for Mental Health, and an anemic percentage of the 2025 total VA budget request of $369 billion. The VA should make veterans’ mental health and suicide prevention its number one overall priority, not just its number one clinical priority. Community organizations are a critical part of addressing this.
As previously mentioned, less than half of veterans in the United States are enrolled in VA care. Some don’t use VA because they have private insurance, others fear going to the VA after all the horror stories they’ve heard, or refuse to use it after a bad experience. Community organizations, particularly in rural areas, may have connections to the veteran community the VA will simply never have.
Additionally, many of the grants have gone to larger organizations. In 2022, for example, 80 Fox Grant awards went to healthcare corporations and state-level organizations.
Smaller organizations often have the ability to form the closest relationships with veterans, and in some cases, they are more likely to know the needs of a specific area or community. And smaller organizations do not typically have as many options for procuring financial support for their programming.
Why is the suicide rate higher among veterans?
The latest VA figures, from 2021, show there were roughly 17 veteran suicides per day, or 6,392 a year; veterans commit suicide at a 57% higher rate than nonveteran adults.

The number of veteran suicides might be even higher than that. One study found that the rate of suicide among veterans could be as much as 37% higher than the numbers reported by the VA.
There are still systemic issues with the VA’s handling of suicide prevention. According to a Mission Roll Call survey, 53% of Americans believe the federal government has “not been very effective” in dealing with suicide among veterans. And 47% believe the government has not been very effective in dealing with transition to civilian life. Tellingly, among Americans who know a service member, those numbers are higher.
The Veterans Crisis Line is a 24/7 helpline (telephone, text messages and online chat) for veterans struggling with suicidal thoughts and mental health. But in September 2023, the Veterans Affairs Office of Inspector General (OIG) issued a “damning” report of how a suicidal veteran was handled by crisis line staff in 2021. The veteran took their own life minutes after their call to the crisis line ended.
OIG found that the crisis line worker failed to transfer the text conversation to a phone call, contact third-party rescue personnel, or confirm that a family member successfully intervened in the patient’s efforts to commit suicide. The suicide prevention program case manager only contacted the sheriff’s department the next day to request a welfare check. By then, it was too late.
This is just one example of the ways current programs are too reactionary. Outreach and funding to local organizations need to dramatically increase in order to catch veterans at a much earlier point in their spiraled crisis.
The risk factors for veteran suicide, in some ways, look similar to the risk factors for nonveterans: financial stress, substance abuse, mental health diagnosis, problems in a romantic relationship, and unemployment. But there’s one additional critical factor among veterans – an abrupt and often overwhelming loss of community and identity.
There is no uniform “exit strategy” for a veteran transitioning to civilian life.
Many veterans are not prepared for the feelings of loss that come when they are ripped away from the only community they have known for years. Military service touches all aspects of life, from housing to healthcare to social life. When you transition from the military, you don’t just leave your job and your salary. You often leave your house, your city, your friends and your purpose. When you add post-traumatic stress from deployment and combat, it can be a difficult transition.
The best way to combat mental health struggles that come from a loss of community is for community to step in. This is why community organizations that understand and address veterans’ issues are so important.
How can we support veterans’ mental health?
Doctor’s appointments, disability benefits and reskilling aren’t enough to tackle the mental health challenges veterans are experiencing. The Department of Defense and the VA need to fundamentally change the way they approach veteran mental health by taking a more holistic approach to the problem. This starts with being more proactive in addressing the issue.
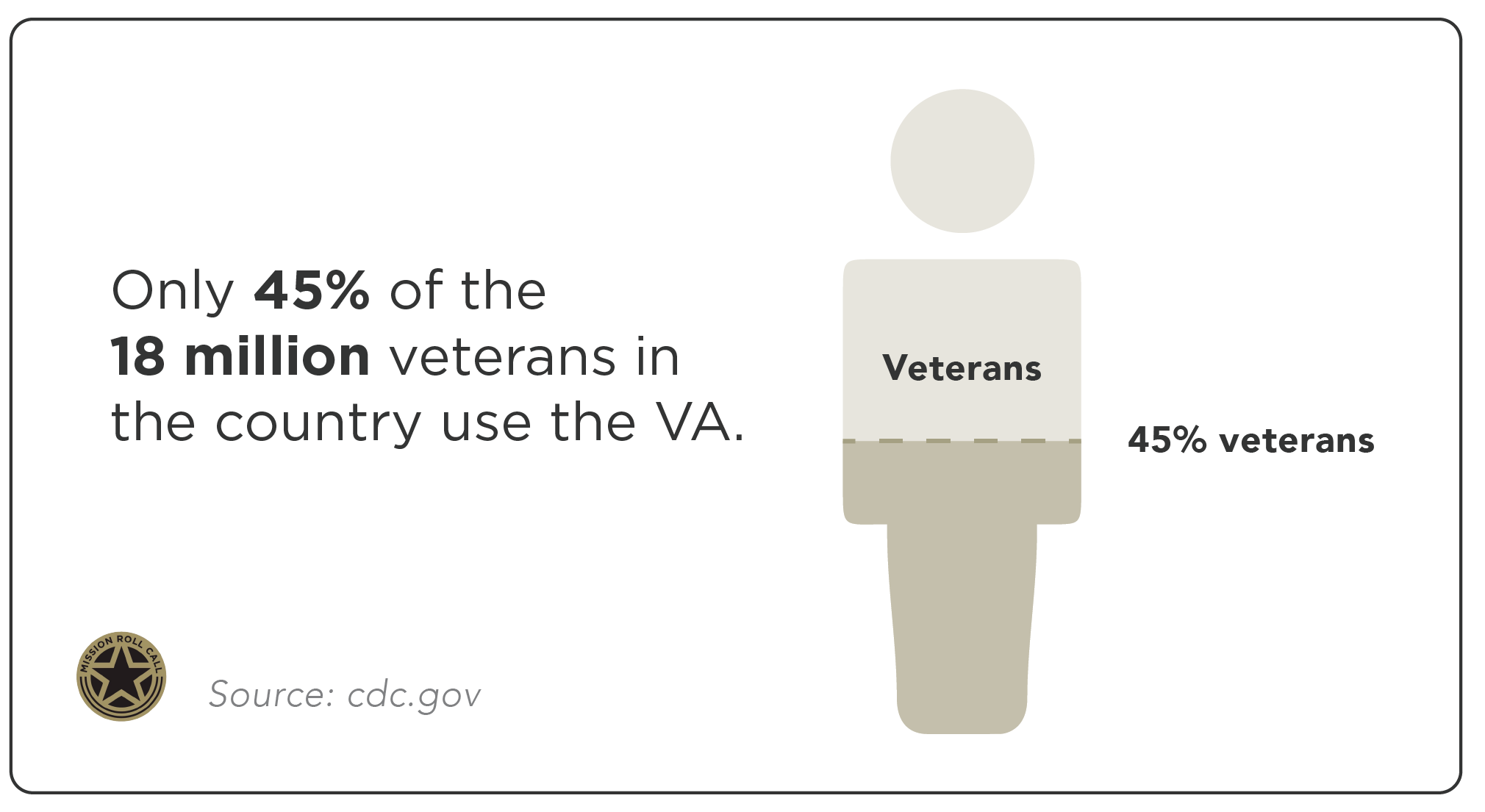
1. Advocate for all veterans, whether or not they’re using the VA.
Only 45% of the 18 million veterans in the country use the VA. The best way to tackle the issue of suicide and mental health among veterans is by advocating for policies that provide services to veterans, whether or not they’re engaged with VA services. That’s why policies that fund community organizations that work with veterans are so important.
Mission Roll Call shares stories and news about policies that affect veterans. We also take the views, experiences and insights shared by our veterans and deliver them directly to our leaders in order to speak unfiltered, accurate truth and enact positive change. If you are a veteran or active duty service member or family member, make your voice heard by participating in our monthly polls.
2. Increase collaboration between government and military branches.
Preventing veteran suicide requires more collaboration among the VA, various branches of the military and the Department of Defense. They still have a lot of joint work to do on meaningful transition assistance and things like electronic health record management to make reintegration into civilian life as seamless as possible.
Veteran suicide should be the top priority for the VA. One way this can be achieved is for the Office of Suicide Prevention to be a direct report to the U.S. Secretary of Veterans Affairs, and not housed under the Office of Mental Health.
3. Support meaningful, local connections.
The more we empower community organizations to go find veterans and to work with them, the more we are able to replace connections that were lost after they transitioned out of the military.
Every year, Mission Roll Call visits geographically diverse, veteran-heavy communities across America. We polled veterans in these communities beforehand and were able to compare places like Dallas that had high approval ratings with places like Los Angeles that had low ones. We found that in areas like Dallas, VA officials, nonprofits, and for-profit companies routinely left their facilities to interact with veterans in their communities. They had networks of highly motivated individuals who would find veterans in need and connect them with the appropriate resources.
We can’t wait for veterans to ask for help. Veteran support organizations need to be proactively engaging and getting to know veterans in order to address any small struggles before they become big ones.
4. Spread the word.
Small but effective organizations may not be aware of grant opportunities that exist. The VA needs to invest resources in targeted awareness of these grant opportunities — especially to the communities that their notice claims to prioritize.
Ensuring the application window is long enough for organizations to sustainably and effectively complete all requirements — and that the organizations have an awareness of these kinds of opportunities — will help promote parity among applicants and put necessary funding into diverse veterans communities in need.
Reach out to your representative in Congress and encourage them to advocate for the veterans in your area.
5. Reach out to veterans.
Members of the community have a vital role to play in supporting veteran mental health. But according to a Mission Roll Call survey, only 35% of American civilians know a veteran, and 13% know someone currently in the military.
There are a number of ways to volunteer with veterans in your community and become part of the support network veterans need. Reach out to organizations in your community.
Mission Roll Call has had the privilege of sitting down to hear from many veteran nonprofit organizations, including America’s Warrior Partnership, Black Ops Rescue, Boulder Crest Foundation, Honor Flight Network and more. Find an organization you can help (through donations, advocacy or volunteering) on Mission Roll Call’s Veteran Nonprofit’s list.
Get to know the veterans in your community. It might save their lives.
Conclusion
Congress and the VA have made strides in the right direction toward preventing veteran suicide, but the job is not done until every veteran has access to the resources they need to save their lives.
Not all wounds are visible. Military personnel can be exposed to an array of potentially traumatizing experiences that can impact them for years and decades in the future. With more than four in ten veterans in need of mental health care programs, we need proactive government and community involvement to heal our veterans.
Mission Roll Call will continue to advocate for meaningful legislation, not just so that all veterans have access to quality care, but that this care actually reaches them.
Veterans in need of emergency counseling can reach the Veterans Crisis line by dialing 988 or 1-800-273-8255 and selecting option 1.
The immense value of military service is not always reflected in veterans’ experiences upon leaving the military. They often face problems related to difficulties in transitioning from military life to civilian life, which can involve navigating complex bureaucracy to accessing benefits; the effects of traumatic or moral injuries; and systemic gaps in mental health services.
Veterans’ common stressors can impact family, social, and professional relationships.
To make matters worse, many civilians may not be aware of or fully understand these unique issues.
Mission Roll Call aims to give veterans a unified voice on issues that matter to them. Through online polls, in-person outreach across the country, and social media, we identify and highlight the unique needs of our country’s veterans to encourage greater support from legislators and among communities.
Here are the seven most common challenges U.S. veterans face:
- Difficulties Transitioning From Active Duty to Civilian Life
- Experiencing PTS and Gaps in Mental Health Support
- Missing the Camaraderie, Community, and Purpose Found While Serving
- Access to Benefits for Underserved Veterans
- Lack of Proper Transportation for Disabled Veterans
- Homelessness
- Being Confronted with Veteran Stereotypes in Entertainment and Civilian Life
1. Difficulties Transitioning From Active Duty to Civilian Life
What difficulties do veterans face when transitioning from the military?
An estimated 250,000 men and women leave or retire from U.S. military service and return to civilian life each year. As of 2023, there were a reported 17.9 million former service members in the U.S. In transitioning to civilian life, navigating the VA healthcare system, finding affordable housing, and applying for jobs can present difficult challenges.

According to a Mission Roll Call poll, 85% of veterans said they felt the military transition assistance program did not prepare them well for leaving military service.
When on active duty, service members receive food and housing assistance along with comprehensive healthcare. The process of securing a job that allows them to provide for their families in the same way and assures the same kind of financial security in a new phase of life is not easy, especially for those with a service-connected disability.
Veterans can experience social and relational challenges with family and friends post-service as well. Shifting from service-related responsibilities to the demands of civilian life and new work environments is a distinct journey that others are not usually able to relate to.
The VA’s Transition Assistance Program, known as TAP, provides tools, information, and resources to service members and their loved ones to help prepare them for the transition to civilian life. Yet its broad approach to aiding veterans is not sufficient preparation in many cases.
Veteran feedback published in the Journal of Veterans Studies underscores this.
Its 2020 article exploring what a successful transition model could look like notes that more attention should be given to adjusting to “new work/educational/cultural settings, meeting family transition needs, financial management issues, procuring housing, dealing with trauma responses, or assuring that veterans truly obtain the benefits and support they need.”
Simply put, veterans would benefit from clear, comprehensive roadmaps and support for this significant life change. The VA must enhance its initiatives and programs to effectively prepare veterans.
2. Experiencing PTS and Gaps in Mental Health Support
Do veterans experience post-traumatic stress at higher rates than non-veterans?
Service members can be exposed to combat and non-combat situations that can negatively impact their mental health. This, along with systemic gaps in mental health care, can cause veterans to experience post-traumatic stress (PTS) symptoms at higher rates than civilians.

PTS has come to be known as the “signature wound” of veterans of the Global War on Terror (GWOT) in particular. The VA reports that 15% of veterans who served in Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF) – in Iraq and Afghanistan, respectively – have experienced PTS symptoms in the past year, and 29% of veterans from these wars will experience PTS at some point in life. Part of the reason is that the GWOT saw a rise in improvised explosive devices (IED) and traumatic brain injury (TBI), which can elevate the risk of PTS and other mental health challenges.
For instance, an estimated 22% of all OIF and OEF combat wounds were brain injuries, which have been associated with issues such as memory loss, anxiety, depression, and fatigue. The high rates of PTS among veterans have also been connected to concerning rates of veteran suicides — though it’s only one of many issues that can contribute to self-harm or suicidal ideation.
For instance, Brown University’s 2021 Costs of War Project found that a significant number of GWOT veterans who have died by suicide did not all serve in combat roles. This suggests that the circumstances leading to their death went beyond the common dangers associated with war and could have been attributed to factors like moral wounds, mental health stigmas, and issues in military culture.
Additionally, there are systemic healthcare gaps that can prevent veterans from getting the care and support they need for PTS and other mental health conditions. RAND Center for Military Health Policy Research data shows that less than half of veterans in need of mental health services receive treatment, and less than one-third of those who do are getting proper evidence-based care.
The Biden administration announced in 2023 that veterans in suicidal crisis can now receive free emergency medical care at any VA or private care facility, even if they aren’t enrolled in the VA system.
This new policy is a step in the right direction. However, no veteran should get to that point. It will take greater coordinated efforts between Congress and the VA to address gaps in veteran mental health care and ensure veterans can receive quality care in a timely manner. Reducing appointment wait times, fixing disparities in rural communities, and expanding community care provisions should be at the forefront of that agenda.
3. Missing the Camaraderie, Community, and Purpose Found While Serving
Do veterans lose their sense of purpose once they leave the military?
Though veteran experiences are wide-ranging and not narrowly defined, transitioning from the military can be one of the most challenging life changes for an individual and family. Many service members have a sense of identity, purpose, and camaraderie wrapped up in being part of the military, and it’s easy for that to feel strained or lost once they leave.
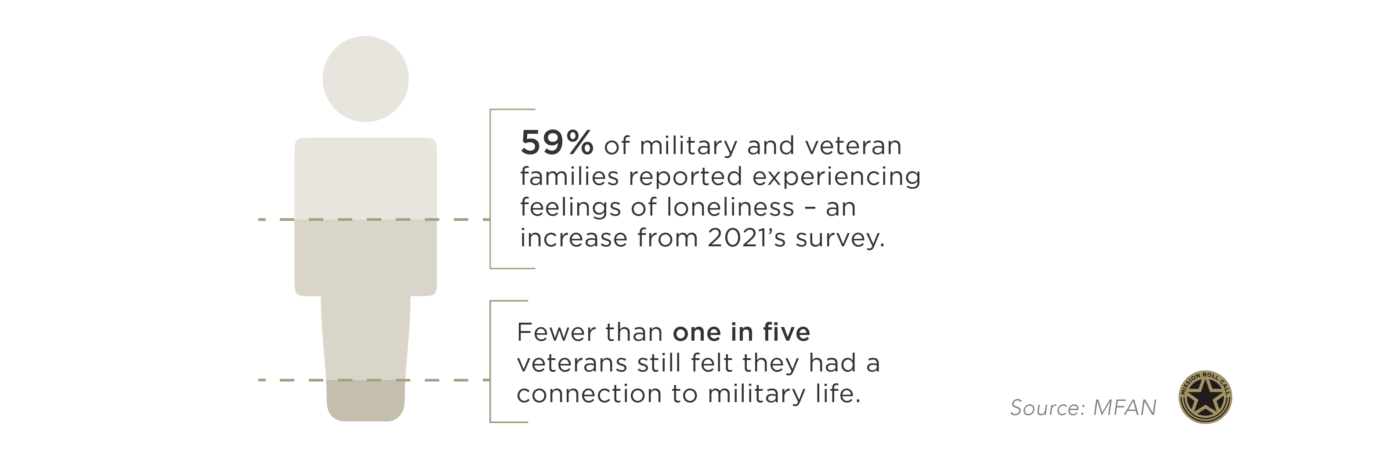
The Military Family Advisory Network (MFAN) surveyed 10,149 military and veteran families for its 2023 report on their quality of life and support. More than 59% of military and veteran families reported experiencing feelings of loneliness – an increase from 2021’s survey. Fewer than one in five veterans still felt they had a connection to military life.
The unique experiences associated with leaving the military can impact service members in several ways. On one hand, there are practical challenges like securing employment, housing, and healthcare benefits, along with social factors that can make this change jarring and complex for veterans. Then there are the socio-emotional shifts: Veterans may find themselves without a sense of purpose and feeling detached from their military community. This can exacerbate the practical difficulties of adjusting to life after service, making it harder to cope with the changes. The military also provides structure that’s not often found in other work environments.
A VA-funded study on veteran social connectedness and its links to depression found that “among five forms of social connectedness, loneliness was tied to the highest levels of depression and suicide ideation, or thoughts of committing suicide. Loneliness was also associated with the lowest levels of patient efforts to manage their health and to seek help.”
In improving assistance for veterans transitioning to civilian life, adequate focus should be placed on the socio-emotional aspects of this major life change. The VA and veteran service organizations should look toward implementing effective ways to foster support systems for service members — such as community initiatives, mentoring, and connection groups — as they shift to this new chapter.
4. Access to Benefits for Underserved Veterans
What challenges do veterans face in accessing their benefits?
More than four million veterans reside in rural communities across the country. Of the more than 18 million United States veterans, nearly a quarter of them – 4.4 million – live in rural areas.
Access to all types of care is important for rural veterans especially because many rural veterans are at an advanced age, with 54% age 65 or older. Additionally, rural veterans are more likely to be diagnosed with diabetes, high blood pressure, obesity, and heart conditions. These conditions require more frequent, ongoing, and costly care.
Among rural veterans are another underserved group – Indigenous veterans, who serve in the U.S. military at higher rates than any other group. There are an estimated 160,000 Indigenous American Indian, Native Hawaiian, and Alaska Native veterans in the United States, and about 39% live in rural areas.
According to the VA, tribal veterans are more likely to lack health insurance and have a disability – service-related or otherwise. Additionally, Native American health is disproportionately worse than other racial groups in the U.S., with extremely high rates of heart disease, diabetes, and cancer.
Providing comprehensive, high-quality care to underserved veterans is a challenge, leading to further health disparities among these communities.
In transitioning to civilian life, veterans can experience significant challenges when navigating the complexities of VA benefits, particularly as it relates to the VA healthcare system.
Blue Star Families’ 2023 Military Lifestyle survey found respondents named access to military/VA health care systems as one of their top concerns.
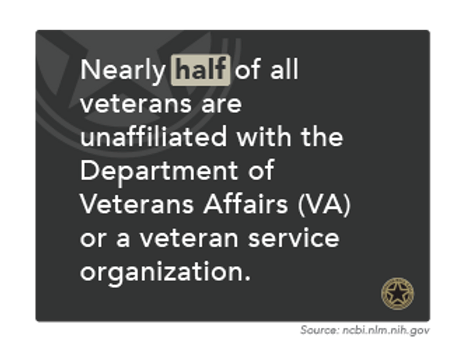
Nearly half of all veterans are unaffiliated with the Department of Veterans Affairs (VA) or a veteran service organization. One of these reasons is because, for many, VA facilities are backlogged or far away.
The VA’s Transition Assistance Program, or TAP, does not adequately prepare veterans for the complexities of securing benefits nor the current pitfalls of VA care, such as long wait times and disparities in rural areas.
In fact, an April 2022 audit from the VA department’s inspector general found data on VA healthcare facilities was being reported inconsistently and in a way that conceals true wait times. And a February 2023 report by the Government Accountability Office (GAO) found that veterans living in rural areas often face unique barriers to accessing mental health care largely due to “staff shortages in rural facilities and transportation issues.”
There have been a few promising legislative steps in recent years. The VA expanded benefits eligibility to over 3.5 million veterans after the PACT Act was passed in August 2022. The VA also launched a mobile application called VA: Health and Benefits, meant to centralize veterans’ health and benefits information. The VA’s Connected Care Program seeks to bring broadband access to more rural places with limited capacity, in order to support remote virtual care.
Still, there’s significant work to be done. The VA must:
- increase awareness and better explain VA benefits prior to service members’ exit from the military;
- reduce wait times for appointments with VA providers and right-size VA inequities in underserved areas; and
- ensure veterans can receive quality care elsewhere when the VA cannot provide it in time or within a reasonable distance.
A 2023 RAND study concluded that “for veterans with limited access to a VHA facility or who are unable to access timely care, community care providers are a potentially important resource.”
Most of all, Congress needs to provide oversight to see that the VA adheres to the guidelines outlined in the Mission Act — aimed at strengthening comprehensive healthcare for all veterans (especially those who suffer proportionately higher rates of health challenges, such as rural and tribal veterans) — and that funds are being allocated effectively.
5. Lack of Proper Transportation for Disabled Veterans
What transportation needs do veterans face, and how can we meet them?
Transportation helps connect veterans to employment, regular health care visits, support services, and other necessities that are vital to a good quality of life. Lack of access to proper transportation or the funds to secure it can be a significant hindrance to veterans accessing their basic needs.
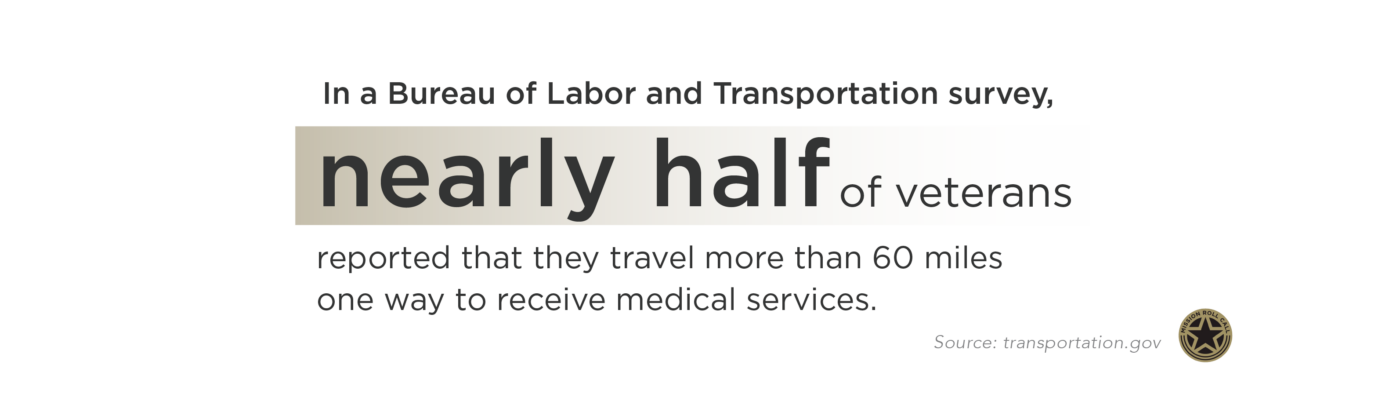
In a Bureau of Labor and Transportation survey, nearly half of veterans reported that they travel more than 60 miles one way to receive medical services.
A considerable number of veterans need specialized transportation as well. There are an estimated 5.27 million veterans — over one-third of the veteran population — who identify as having a disability that requires transportation assistance.
It’s critical that veteran benefits include comprehensive transportation assistance, especially for veterans with a service-connected disability.
In a promising step, the AUTO Act was also signed into law in early January 2023, allowing disabled veterans who need modified vehicles to receive a grant from the VA every 10 years rather than once in a lifetime.
Nevertheless, additional efforts are needed by Congress and the VA to ensure all veterans have access to proper transportation and are aware of the transportation benefits available to them. This should include periodic follow-up with recently transitioned veterans, awareness campaigns around benefits, and a review of funding allocation for veteran transportation assistance.
6. Homelessness
Do veterans experience higher rates of homelessness than nonveterans?
Veterans have a higher likelihood than nonveterans of becoming displaced from their homes. Veteran homelessness is one of the top issues of concern for U.S. veterans. In a Mission Roll Call poll of veterans nationwide, more than 90% of veterans said they do not think enough is being done to address veteran homelessness.
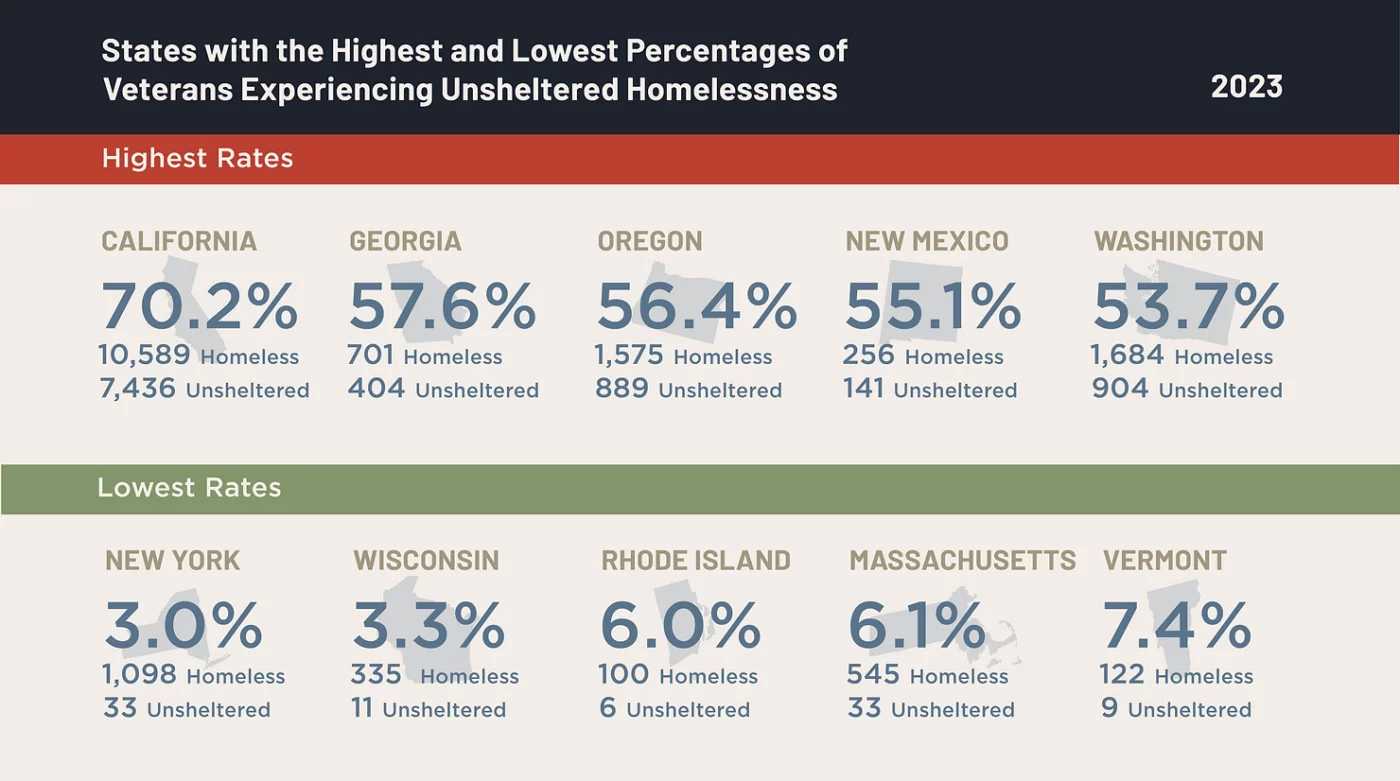
The number of homeless veterans is increasing – rising more than 7% from 2022 to 2023. On an average night in 2023, 20,067 veterans were living in shelters. A staggering 15,507 veterans were living without any shelter at all.
There are also racial disparities. Black veterans are significantly overrepresented among homeless veterans, making up 31% of the homeless veteran population (but only 14% of the overall veteran population).
A number of interconnected factors are contributing to the rise in veteran homelessness, including gaps in mental health support and the growing disparity between housing costs and income.

Government efforts to solve this crisis are being made. In 2024, the Department of Veterans Affairs set goals to permanently house at least 41,000 homeless veterans and ensure that 95% of them do not return to homelessness within the year. Also in 2024, Housing and Urban Development announced nearly $3.16 billion in Continuum of Care program awards for over 7,000 projects that provide housing assistance and/or supportive services to people experiencing homelessness.
However, over $50.3 billion has been collectively spent on government programs since FY2005. Yet, veteran homelessness and hunger persist. It’s clear that money alone is not enough to fix this problem.
Mission Roll Call advocates for more funding for community-based nonprofits and businesses that are on the frontlines of many veterans’ services. These services don’t just address homelessness specifically but also target the root causes of homelessness. These community organizations have touchpoints in the veteran community that the VA will never have.
7. Being Confronted with Veteran Stereotypes in Entertainment and Civilian Life
What are the common stereotypes about veterans, and how can we address these?
There are several stereotypes and misconceptions that can negatively impact the daily lives of veterans. A 2021 study by the University of Cincinnati looked at common stigmas veterans face. Through in-depth interviews with veterans ages 20 to 60, it found that “depictions of veterans in news media and pop culture often carry negative associations such as poor mental health or violence.”
Respondents shared that “views about military personnel are skewed by war movies that depict returning veterans as psychologically damaged by their experience” and many believed these portrayals can lead to “inappropriate and off-base comments by civilian peers.”
Yet veterans have lower unemployment rates than nonveterans, as of July 2024.

Veterans are also more likely to be civically engaged than non-veterans, and on average, veterans contribute more volunteer time in their communities than non-veterans.
And while the majority of Americans look up to people who have served in the military, there are still negative misconceptions that have permeated society.
Adding to this, and unlike other high-stress occupations such as law enforcement, medicine, or emergency response roles, veterans who enter the workforce usually aren’t surrounded by people with similar experiences and perspectives. This contributes to gaps in understanding, and they can be met with unrealistic or unfair assumptions about their capabilities.
These portrayals and misconceptions can have serious implications on veterans’ mental health, careers, social lives, and overall well-being. Workplaces, entertainers, and everyday people should be mindful of the inaccurate stereotypes impacting veterans and do all that’s within our power to put an end to them.
Bottom Line:
While some challenges for veterans may be obvious and widely discussed, there are stressors that the average person is not unaware of. As individuals, we can show support to veterans by educating ourselves on their unique needs and challenging harmful stereotypes or stigmas. We can also volunteer with veteran nonprofits and point former service members to useful benefits, service organizations, social groups, and other resources.
Mission Roll Call is dedicated to advocating for action on each of these issues in 2024 and beyond. Through outreach, polling, storytelling, and media, we present the concerns of veterans across the country to leaders in Washington. Collectively, we can urge Congress and the VA to address these unique stressors veterans face by sending letters or emails to our congressional representatives. Join us to add your voice to the conversation.
It’s time for effective solutions to these solvable issues. We must ensure our courageous veterans and their families have access to the benefits they’ve earned and the basic essentials for a good quality of life.
Veteran homelessness remains a critical issue in our country, affecting countless veterans and their families. At Mission Roll Call, our members have identified this challenge as a top priority for advocacy.
Today, we are honored to share exclusive messages from Senator Jon Tester and Senator Mike Bost, co-chairmen of the Veterans’ Affairs Committee, who discuss the urgent need for action and the steps being taken to address this crisis. These videos provide valuable insights into the current state of veteran homelessness and the ongoing efforts to support our nation’s heroes.
To deepen your understanding of the challenges and solutions, we invite you to read our comprehensive piece, The State of Veteran Homelessness.
By sharing your voice and becoming a member of Mission Roll Call, you can help us advocate for meaningful change and support initiatives that ensure every veteran has a safe place to call home. Together, we can make a difference. Let your voice be heard by subscribing here.
The number of homeless veterans is increasing – rising more than 7% from 2022 to 2023. On an average night in 2023, 20,067 veterans were living in shelters. A staggering 15,507 veterans were living without any shelter at all.
Veteran homelessness is one of the top issues of concern for U.S. veterans. In a Mission Roll Call poll of veterans nationwide, more than 90% of veterans said they do not think enough is being done to address veteran homelessness.
Solving this issue is complex, and requires on-the-ground solutions as well as political action. That’s why Mission Roll Call is committed to increasing awareness of veteran homelessness among policymakers and to advocating for concrete solutions on Capitol Hill, including understanding and addressing the root causes.
This article will address the following questions:
- Are veterans at higher risk of homelessness than nonveterans?
- What is contributing to the increase in homelessness among veterans?
- How does being homeless affect veterans?
- What is the U.S. government doing to address homelessness?
- What resources are available to homeless veterans?
- What can you do to help veterans who are experiencing homelessness?
Are veterans at a higher risk of homelessness than nonveterans?
Veterans have a higher likelihood than nonveterans of becoming displaced from their homes. They make up about 7% of all homeless adults in the U.S., even though they only represent around 6% of the total U.S. population.

Homelessness includes what is known as “sheltered homelessness” – housing in an emergency shelter, transitional housing, or a safe haven program – as well as “unsheltered homelessness” – living and sleeping in places not meant for human habitation. Troublingly, from 2022 to 2023, the number of unsheltered veterans rose 14%.
The recent increase in homelessness among veterans is a troubling and newer trend. From 2010 to 2022, the number of veterans experiencing displacement decreased by over 50%, according to the U.S. Department of Urban and Housing Development.
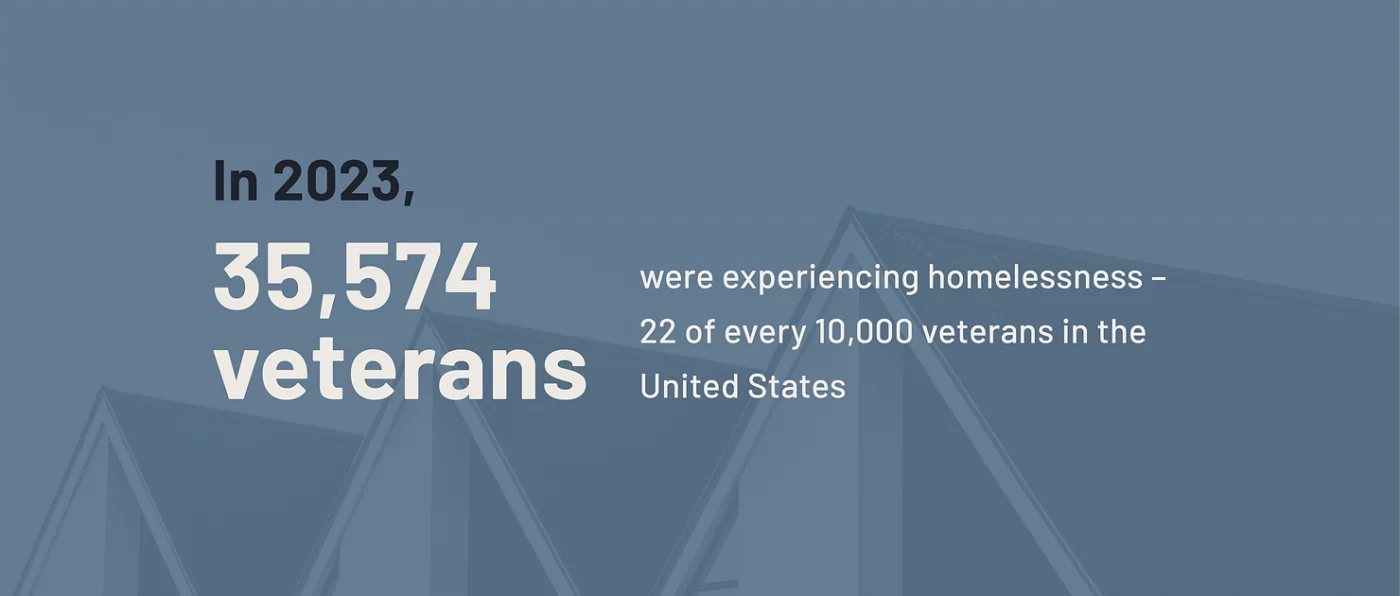
In 2023, 35,574 veterans were experiencing homelessness – 22 of every 10,000 veterans in the United States – compared to 20 out of every 10,000 nonveterans experiencing homelessness in 2023. Just over half of these veterans were staying in sheltered locations, according to the Department of Housing and Urban Development (HUD).
In addition, there are certain groups among homeless veterans that are disproportionately affected. Men make up about 88% of homeless veterans, while female veterans are more likely to be homeless with children – highlighting the need for family-specific support.
There are also racial disparities. Black veterans are significantly overrepresented among homeless veterans, making up 31% of the homeless veteran population (but only 14% of the overall veteran population). And geographically, the risk of homelessness among veterans varies. California, Florida, and Texas have some of the highest concentrations of homeless veterans, with California alone accounting for 30% of all homeless veterans in the U.S.
What is contributing to the increase in homelessness among veterans?
It is difficult to pinpoint any one root cause of the veteran housing crisis; rather, it is an accumulation of factors over time.
Mission Roll Call has outlined several common challenges veterans face. These challenges can be closely linked with homelessness:

1. Difficulties transitioning from active duty to civilian life
In transitioning to civilian life, navigating the VA healthcare system, finding affordable housing, and applying for jobs can be a difficult and drastic shift. According to Pew Research Center, only one in four veterans has a job lined up after leaving the military. And a survey conducted by Prudential found that more than two-thirds of veterans consider finding a job to be the greatest challenge in their transition to civilian life.
2. Gaps in mental health support
Mental health conditions are prevalent among homeless veterans. According to the National Health Care for Homeless Council, pre-existing conditions are exacerbated by the stress and instability of homelessness. As a result, many homeless veterans resort to substance use as a coping mechanism, which further deteriorates their health.
The World Health Organization reports that people suffering from severe mental health issues face additional barriers to employment. But there are systemic healthcare gaps that can prevent veterans from getting the care and support they need for mental health conditions.
3. Navigating VA bureaucracy for access to benefits
Nearly half of all veterans are unaffiliated with the Department of Veterans Affairs (VA) or a veteran service organization. Those who are may face long wait times and fail to get the care they need in a timely manner.
4. Legal difficulties
Many homeless veterans don’t have identification or legal documentation like a driver’s license or birth certificate. Lacking identification prevents them from being able to access many services and programs. Additionally, without an address to receive tickets or other legal paperwork, veterans who have unpaid fines, or have been arrested for a misdemeanor may miss court dates, triggering a warrant.
5. Service-related disabilities
About 30% of veterans had a service-connected disability in 2023, and an estimated 5.25 million veterans identify as having a disability that requires transportation assistance. These disabilities can impact mental health and make it harder to find stable employment.
According to the VA, other factors impacting veteran homelessness include:
6. The growing disparity between housing costs and income
Income inequality drives hundreds of people into homelessness on any given night in dozens of communities across the U.S. Many veteran households face a housing cost burden, spending a large portion of their income on housing. Female veterans, in particular, tend to have lower incomes and are less likely to own homes, making them more vulnerable to homelessness.
7. Substance abuse
Opioid abuse is a growing and critical problem for veterans. Homeless veterans are more likely to have opioid addiction, according to the VA’s Center for Health Equity Research and Promotion. Additionally, veterans who are diagnosed with a drug use disorder are more than twice as likely to become homeless as others.
How does being homeless affect veterans?
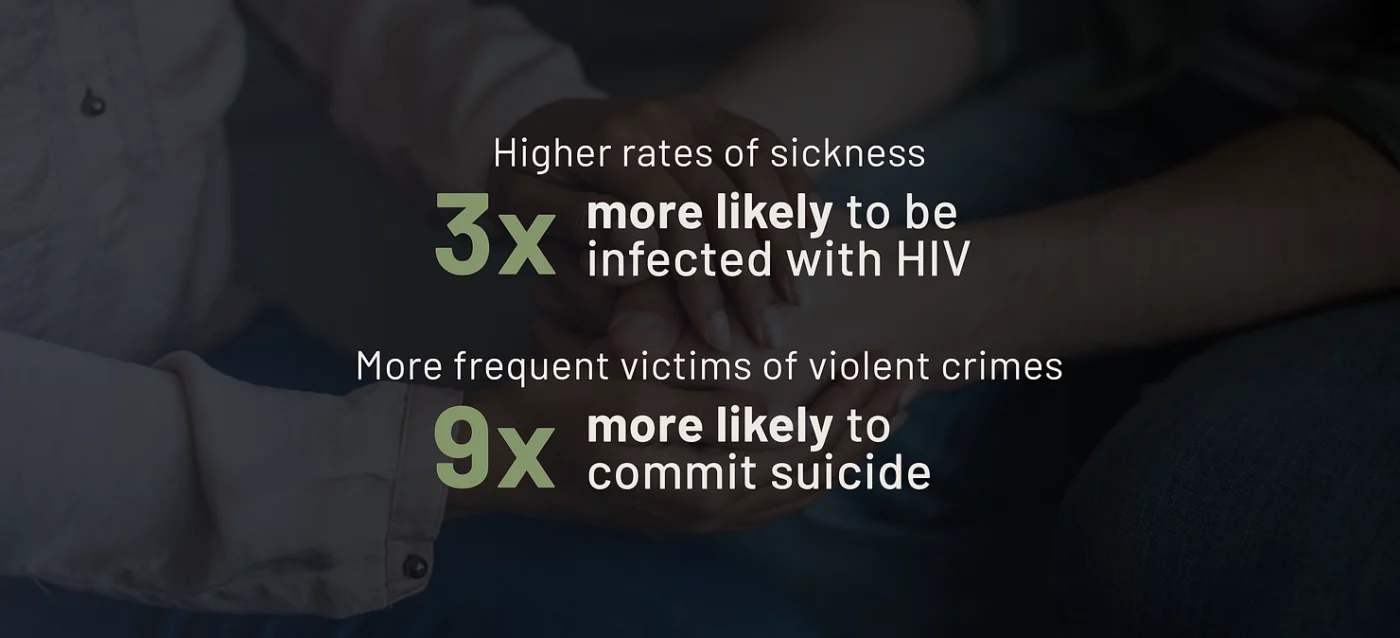
Homelessness significantly worsens veterans’ health, both physically and mentally. A National Health Care for Homeless Council study depicts that the homeless have higher rates of illness and die on average 12 years prior to housed Americans.
Homeless veterans are three times more likely than the rest of the U.S. population to be infected with HIV. They’re also more likely to be in need of dental care. Dental problems, like missing teeth, can be “tremendous barriers” to looking for and finding work.
Research also shows that homeless individuals are more frequently victims of violent crimes than the general population. Between 2020 and 2022, the National Coalition for the Homeless tracked nearly 2,000 violent incidents targeting homeless individuals.
The trauma of homelessness can also lead to increased suicide rates among homeless veterans. Suicide rates among homeless populations are estimated at nine times that of the U.S. general population.
What is the U.S. government doing to address homelessness?
The U.S. government has implemented several initiatives to combat veteran homelessness, focusing on both immediate housing solutions and long-term support services.
In 2024, the Department of Veterans Affairs set goals to permanently house at least 41,000 homeless veterans and ensure that 95% of them do not return to homelessness within the year. They also plan to engage with 40,000 unsheltered veterans to provide them with housing and essential services.
Each year, HUD awards Homeless Assistance Grants to communities that provide housing and related services at the local level – which is critical to reaching veterans who don’t use VA services. In January 2024, HUD announced nearly $3.16 billion in Continuum of Care program awards for over 7,000 projects that provide housing assistance and/or supportive services to people experiencing homelessness.
The administration also launched initiatives like the Housing and Services Partnership Accelerator, which helps states coordinate housing and health services for homeless individuals. This initiative helps fulfill goals stated in All In: The Federal Strategic Plan to Prevent and End Homelessness, which aims to reduce homelessness by 25% by January 2025.
Additionally, the VA is conducting research into innovative ways to increase homeless veterans’ access to care. For example, they have found that peer mentors can play important roles in homeless veterans’ lives. Another finding is that integrating legal aid with medical care improves both mental health and housing – and may help reach veterans who do not use the VA for medical care. A study published in 2017 found that veterans’ mental health and housing situation improved when they accessed free legal services in a VA facility.
What resources are available to homeless veterans?
There are four different federal agencies (the Departments of Veterans Affairs, Agriculture, Labor and Housing and Urban Development) that fund more than ten different homelessness and food insecurity programs, including SNAP and the VA/HUD voucher program, to fight homelessness in the veteran community.
Examples of VA programs include:
- The HUD-VA Supportive Housing (HUD-VASH) program provides rental assistance and case management services to veterans.
- Homeless Patient Aligned Care Teams (HPACTs) provide medical care, mental health treatment, and case management services.
- The VA’s Legal Services for Veterans (LSV) program helps veterans with issues such as eviction prevention, accessing public benefits, and resolving other legal matters that impact their housing stability.
In total, over $50.3 billion has been collectively spent on government programs since FY2005. During that same period, health care obligations for homeless veterans reached $7.8 billion annually in fiscal year 2020, and $700 million for homeless-veteran programs was included in COVID-19 relief packages. Yet, veteran homelessness and hunger persist.
It’s clear that money alone is not enough to fix this problem. Mission Roll Call is pushing for more funding for community-based nonprofits and businesses that are on the frontlines of many veterans’ services. These services don’t just address homelessness specifically but also target the root causes of homelessness. These community organizations have touchpoints in the veteran community that the VA will never have.
For example, The Boulder Crest Foundation focuses on post-traumatic growth, offering programs and retreats designed to help veterans and their families build resilience and thrive in their civilian lives. Team Red, White and Blue connects veterans through physical and social activity.
America’s Warrior Partnership connects veterans and their families with local, regional and national resources. And U.S. VETS provides housing, mental health programs, career services, and more, serving more than 5,500 veterans and families across the country every night.
What can you do to help veterans who are experiencing homelessness?
Without proper community and government support, many veterans struggle to maintain stable housing. Even one veteran experiencing homelessness is too many in a nation that prides itself on service. Support for veterans has to start early, including paying active duty military – especially junior enlisted – the necessary salaries they need to live, thrive and save for their futures.
Mission Roll Call provides veterans with a powerful, unified voice that is heard by our nation’s leaders. Veterans have spoken: veteran homelessness needs to be a top priority for our government.
Here’s how you can make a difference:
- Support Mission Roll Call, which advocates for legislation to help homeless veterans.
- Donate to organizations and nonprofits that provide essential services such as housing, healthcare, and job training to veterans. Mission Roll Call has published a list of some vetted nonprofits.
- Volunteer at local shelters, VA facilities, or organizations that support veterans experiencing or at risk for homelessness.
- If you’re an employer, consider hiring veterans. Their skills and experiences are valuable, and providing employment can help them transition to stable living.

It’s important to advocate for legislative action by writing to your senator about bills that aim to improve housing and services for veterans. One issue that needs reform is that currently, landlords who use funding from government programs have little incentive to permanently fix the problem of homelessness, since getting veterans into permanent housing from temporary housing means the loss of federal funding.
These federal programs do help, but the number of veterans still struggling to find permanent solutions to housing problems makes clear that our current systems are not enough.
Importantly, research has found that Americans have become more compassionate toward the homeless in recent years. These findings, alongside legislative attention and increased public awareness of the issue of veteran homelessness, are important steps for ending veteran homelessness in the United States.
At Mission Roll Call, we believe in the power of veterans and their families to continue serving their communities. That’s why we’re proud to support Vet the Vote, a national initiative dedicated to encouraging veterans and military family members to become poll workers. Their mission aligns perfectly with ours: to give veterans a voice and ensure their continued contribution to our democratic processes.
This year, Vet the Vote traveled the country, encouraging service members and their families to take on this vital role. Recently, they were at the Raider’s stadium in Las Vegas for a Day of Gratitude, engaging with over 20,000 veterans and military family members. Next week, Vet the Vote is excited to host two more events in Georgia.
Join us to hear from the Vet the Vote team, state and local elections officials, and fellow veterans about the importance of serving as poll workers. These events are open to veterans and military family members, but space is limited, so be sure to RSVP using the links below.
Vet the Vote – Paulding County Event
- Date: Tuesday, July 16
- Time: 2:00pm – 3:00pm EST
- Location: Paulding County Elections Office, 240 Constitution Boulevard Dallas, GA 30132
- RSVP Here: Eventbrite – Paulding County
Vet the Vote – Muscogee County Event at the National Infantry Museum
- Date: Wednesday, July 17
- Time: 2:00pm – 3:00pm EST
- Location: National Infantry Museum, 1775 Legacy Way, Columbus, GA 31903
- RSVP Here: Eventbrite – Muscogee County
We look forward to seeing you there and continuing our joint mission to support veterans and their families in making a difference.
For many veterans and their families, the shift from military service to civilian employment can be challenging. Annually, about 200,000 service members join the veteran community, with nearly half leaving their first civilian job within a year and around 80% within two years.
They deserve better.
“Transitioning from military service to civilian employment is a crucial step for veterans and their families,” said Jim Whaley, CEO of Mission Roll Call. “It’s essential for all organizations to support veterans in finding meaningful employment that challenges them and provides a sense of purpose similar to their military service. Our veterans have unique skills and experiences, and it’s our collective responsibility to help them translate those into fulfilling careers.”
Fortunately, numerous veteran service organizations are dedicated to assisting veterans and military spouses in finding meaningful employment and successfully navigating this transition. Here, we highlight some of the top veteran service organizations providing invaluable resources and support for veterans seeking employment.

USO Pathfinder Transition Program
The USO Pathfinder Transition Program offers comprehensive transition services to active-duty service members, National Guard members, reservists, and military spouses.
The program provides personalized support, including career counseling, resume-writing assistance, and networking opportunities. Pathfinder Scouts guide participants through various aspects of their transition, helping them achieve their employment and education goals.

The Honor Foundation
The Honor Foundation is a unique organization that specializes in assisting Navy SEALs and other special operations forces transition to the civilian workforce. Their program includes a three-month intensive curriculum focusing on career development, personal branding, and networking.
The Honor Foundation also offers executive coaching and access to a vast network of mentors and employers dedicated to helping veterans find fulfilling careers.
USA Jobs for Veterans
USA Jobs for Veterans is an official website of the U.S. government, designed to help veterans find federal employment opportunities.
The platform provides a wide range of job listings, application tips, and resources tailored to veterans. With a focus on matching veterans’ skills and experiences with appropriate federal positions, USA Jobs for Veterans is a valuable resource for those seeking government employment.

Wounded Warrior Project
The Wounded Warrior Project (WWP) offers several programs aimed at helping veterans transition to civilian employment. Their Warriors to Work program provides career counseling, resume assistance, and job placement services. WWP also hosts career fairs and networking events, connecting veterans with potential employers and offering ongoing support throughout the employment process.

Hire Heroes USA
Hire Heroes USA is dedicated to empowering U.S. military members, veterans, and military spouses to succeed in the civilian workforce. They offer personalized career coaching, resume writing assistance, and job search support.
Their services are free of charge and tailored to meet the unique needs of each veteran, ensuring they are well-prepared for their job search and career transition.
Vets in Tech
Vets in Tech supports veterans by providing them with the resources, skills, and opportunities needed to enter the technology sector. They offer training programs, workshops, and networking events focused on tech careers.
Vets in Tech also partners with leading tech companies to provide job placement assistance and mentorship, helping veterans leverage their skills in the rapidly growing tech industry.

Bunker Labs
Bunker Labs is a national nonprofit organization dedicated to helping veterans and military spouses start and grow their own businesses. They offer a range of programs, including entrepreneurial training, mentoring, and networking opportunities.
Bunker Labs provides veterans with the tools and support needed to succeed in the business world, fostering a community of veteran entrepreneurs who can share experiences and support one another.

Gallant Few
Gallant Few aims to reduce veteran isolation and support successful transitions by connecting veterans with mentors, resources, and communities. Their STAR (Service, Transition, and Reintegration) program offers personalized mentorship and career guidance, helping veterans navigate the challenges of civilian employment.
Gallant Few also focuses on improving veterans’ overall well-being, emphasizing the importance of a holistic approach to transition.
Finding Your Tribe: The Importance of Community with Team Rubicon
In addition to finding employment, many veterans seek a sense of community and belonging after leaving the military. Team Rubicon provides an excellent example of how veterans can find their tribe while making a positive impact. Team Rubicon unites veterans with first responders to deploy emergency response teams, leveraging their skills and experiences to help communities in need. By participating in disaster relief efforts, veterans can regain a sense of purpose, camaraderie, and identity.
The importance of finding a supportive community cannot be overstated. Engaging with organizations like Team Rubicon helps veterans build strong social networks, which can lead to better mental health, increased job satisfaction, and overall well-being. These connections provide a support system that extends beyond employment, offering veterans and their families a foundation for a successful and fulfilling post-military life.
Transitioning to civilian employment is a significant milestone for veterans, their spouses, and families, and having access to the right resources can make all the difference. The organizations highlighted above provide essential support, guidance, and opportunities for veterans seeking to navigate this transition. By leveraging these resources and finding a supportive community, veterans and their loved ones can achieve their career goals and build a successful post-military life.
For more information on these organizations and other valuable resources, read more of our news and stories and explore the support available to veterans and their families.
Introduction
After witnessing or experiencing a traumatic or tragic event, individuals may develop a condition known as Post Traumatic Stress (PTS). Due to the high demands of military service, especially during active wartime deployment, PTS is more likely to develop in veterans than in nonveterans. Service members are often exposed to prolonged periods of stress, life-threatening situations, combat environments, and moral injury following war, all of which can increase the likelihood of developing PTS. Unlike a one-time traumatic event, military trauma can be progressive, making recovery more complex and requiring long-term support.
Some organizations, including Mission Roll Call, choose to use the term post-traumatic stress (PTS) instead of PTSD to help reduce the stigma often associated with the word “disorder.” While “PTSD” is a clinically recognized diagnosis, the term “disorder” carries negative connotations that imply something is inherently wrong or broken, which may discourage individuals from seeking support. This shift in language challenges the stereotype of “broken veterans” and normalizes conversations around mental health without shame. As many veterans emerge from trauma with increased resilience, stronger relationships, and a renewed sense of purpose, MRC incorporates the concept of post-traumatic growth (PTG) to offer a fuller, more hopeful look at the future.
Therefore, PTS will be used throughout the rest of this article (and in all MRC messaging) to promote a more understanding and supportive narrative around veteran mental health.
What is PTS, and what are its indicators? Recognizing these signs is often the first step in treatment and Posttraumatic Growth (PTG). Symptoms may include:
- Flashbacks — recalling memories of the traumatic event, often suddenly and unexpectedly
- Trouble sleeping — struggling with insomnia or sleep quality due to frequent nightmares about the traumatic event
- Avoidance — avoiding places, activities, people, or even conversations associated with the trauma
- Physical reactions — exhibiting physical signs of stress, such as a racing heart, sweating, or an exaggerated startle reflex
- Changes in behavior or personality — irritability, anger outbursts, fatigue, depression, anxiety or nervousness, loss of appetite, sleep problems
- Persistent negative feelings — like shame, guilt, fear, or detachment
- Reckless and self-destructive behavior — acting without thought for one’s own safety
PTS is a condition that can affect anyone who has experienced a traumatic event; however, veterans are at a significantly higher risk than the general public due to the unique and often intense stressors of military service. It’s important for veterans to know that they are not alone, their experiences are valid, and there is help available.

What has changed?
New data from 2024 and 2025 highlights the ongoing mental health crisis among U.S. veterans, especially those with PTS. Veterans diagnosed with PTS face a suicide rate of 51.3 per 100,000, nearly double that of those without the condition. Additionally, mental health and substance use disorders significantly elevate risk, with female veterans experiencing a suicide rate 92% higher than civilian women and male veterans 44% higher than civilian men.
Despite these troubling trends, federal action shows promise. The VA’s 2025 budget proposal has reached $369.3 billion, more than eight times its 2001 level. This includes a significant investment in mental health with an allocated $17 billion in mental health services alongside $583 million for suicide prevention outreach, backed by targeted staffing programs to ensure timely, high-quality care for veterans. Additionally, a new executive order launched the National Center for Warrior Independence, aiming to house 6,000 veterans by 2028 while offering integrated mental health, housing, and job support. Additionally, veteran homelessness decreased by 7% between 2023 and 2024, showing an 11.7% reduction in veterans experiencing homelessness since 2020 and a 55.6% reduction since 2010.
Yet funding alone won’t fix the crisis. These resources must translate into consistent, trauma-informed care, especially for PTS. As suicide rates remain high, the path forward demands centering veterans’ mental health, expanding access, and ensuring support systems deliver real impact beyond policy headlines.

PTS by the numbers
PTS affects veterans across all demographics, but certain groups, particularly post-9/11 veterans and women, are disproportionately impacted. Among veterans who served in Iraq and Afghanistan, the VA estimates that approximately 15 out of every 100 currently live with PTS, with lifetime rates approaching 29%.
Furthermore, women veterans experience PTS at nearly double the rate of their male counterparts, about 13% compared to 6%. These disparities underscore just how essential it is for federal policy, VA systems, and all parts of the veteran support network to adapt in order to meet the full spectrum of mental health needs among those who served.

Continued Change Is Happening
There’s growing momentum in Washington to strengthen how post-traumatic stress (PTS) is identified, treated, and supported. The passage of the Elizabeth Dole 21st Century Veterans Healthcare and Benefits Improvement Act in early 2025 expanded home- and community-based care opportunities for veterans, including provisions for caregiver wellness and support.
Drawing upon this momentum, several bills have been introduced in Congress in the first months of 2025 to better serve veterans and provide for post-traumatic growth.
- H.R. 1290 – Veterans Mental Health Crisis Referral Enhancement Act
- Introduced in February 2025, this bill would increase mental health care accessibility by launching a pilot program in which the VA must provide veterans experiencing mental health emergencies with referrals to approved non-VA mental health care providers.
- Building Resources and Access for Veterans’ Mental Health Engagement (BRAVE) Act
- Introduced in April 2025, this bill looks to strengthen the mental health workforce, infrastructure, and services provided by the VA by taking actions such as extending the Fox Gordon Suicide Prevention Grant Program and improving veteran outreach efforts by vet centers.
- H.R. 72 – TBI and PTSD Treatment Act
- Introduced in January 2025, this bill aims to provide hyperbaric oxygen therapy to veterans with TBI (traumatic brain injury) or PTSD through the Veterans Community Care Program.
What treatments and resources are available to veterans experiencing PTS?
Veterans experiencing PTS have access to a range of evidence-based treatments and resources through the VA and affiliated programs. The VA offers therapies such as Cognitive Processing Therapy (CPT), Prolonged Exposure (PE), and Eye Movement Desensitization and Reprocessing (EMDR), which are proven to reduce PTS symptoms. Veterans can receive care in person at VA medical centers or remotely through VA Telehealth and the VA Video Connect app. For those not ready for traditional therapy, the VA also provides peer support groups, mindfulness programs, and mobile apps like PTS Coach. Additionally, the Veterans Crisis Line (dial 988, then press 1) provides 24/7 confidential support.
Veterans and their families can also explore local and national support options through Mission Roll Call’s Resource Directory, which includes vetted programs that address mental health, transition services, and more. Are we missing a resource you or someone you know has used? Share it with us here.
What work still needs to be done?
While legislative progress continues to be made to support veterans with PTS, there is still important work to be done. Beyond outreach and resources specifically dedicated to addressing it, there is a need for support for the aspects of veteran life that can be made more difficult with PTS.
For instance, the transition from military to civilian life can be difficult, especially if a veteran is suffering emotional or mental strain. Veterans may also face hurdles such as housing, food security, or employment after service. According to a 2022 Mission Roll Call survey, nearly 50% of respondents believe the government has not been effective in dealing with the transition to civilian life.
While there are resources to help with reintegration into civilian life, new or continued support for veterans is critical as they navigate civilian life after their deployment. Ensuring veterans have access to resources that eliminate these burdens is essential for long-term well-being and post-service success.

How can we help?
For nonveterans looking to support those suffering from PTS, there are a number of ways that you can contribute.
For those with a veteran in their life:
- Educate yourself on PTS – Being able to recognize symptoms can be a powerful tool for helping when things get tough.
- Provide support – Let veterans in your life know that you’re there for them if they want to speak about their experiences.
- Know your toolkit – Sometimes people need more than a listening ear. Be aware of available mental health services and encourage them to speak to a professional when needed.
- Connect them with others – Community is necessary for all of us. Encourage them to establish relationships with other veterans and veteran organizations.
If you don’t have a veteran in your life and still want to serve, there are additional ways you can contribute
- Connect with your local VFW or American Legion to see if you could provide a home-cooked meal or provide transportation to medical appointments for a veteran.
- Volunteer or donate to USO lounges, which are at more than 50 airports in the U.S. and tend to be in need.
- Consider donating financial or social media support to Mission Roll Call as we advocate for changes to help care for and support veterans. Donating or volunteering with nonprofits that we’ve vetted and approved could help change a veteran’s life.
Conclusion
Post Traumatic Stress has a profound impact on millions of veterans’ lives every day. As it is understandable and treatable, recognizing the signs, whether emotional, behavioral, or physical, is a critical first step toward healing. With the proper support, including professional treatment, peer networks, and access to veteran-specific resources, those affected by PTS can begin a path toward recovery and even experience post-traumatic growth. No veteran should suffer in silence; help is available, and healing is possible.
June is PTSD Awareness Month, a time dedicated to raising awareness about the impact of posttraumatic stress and the pathways to recovery. In this special Q&A, we delve into the work of the Boulder Crest Foundation, an organization dedicated to transforming the lives of veterans through innovative programs that promote Posttraumatic Growth (PTG).
Experiencing trauma can have a profound impact on an individual’s life, leading to the development of post-traumatic stress (PTS) which can challenge one’s mental, emotional, and physical well-being. However, within the shadows of PTS lies an equally powerful phenomenon: posttraumatic growth.
Mission Roll Call spoke with Josh Goldberg, Chief Executive Officer at the Boulder Crest Foundation, to explore the complex interplay between these two trauma outcomes, identifying how individuals cope with their past experiences and transform them into catalysts for positive change and personal growth. Continue reading to see how the Boulder Crest Foundation is pioneering new ways, and building upon long-standing concepts, to support our heroes and their loved ones.

MRC: Thank you for being part of this conversation, Josh. Tell us about the Boulder Crest Foundation and your approach to posttraumatic growth.
The short version of posttraumatic growth is the idea that what doesn’t kill us can make us wiser and can make us stronger. Posttraumatic growth may seem like a new idea but it’s actually the oldest idea on earth – the idea that in our lives, we will go through great difficulties, and those difficulties will reveal parts of ourselves we won’t know in any other way. Because of those experiences, we can live a more meaningful, authentic, and purposeful life.
The overriding focus for any kind of effort for people who are struggling tends to be, ‘Let’s help these people feel less bad. They’re in pain, let’s give them some measure of relief.’ To us, you essentially sedate or anesthetize people to life. You take them out of the act of living and put them in survival mode.
Our view of suicide is that the opposite of suicide is a life worth living, and a life worth living is filled with purpose and hope, connection and service, and growth. Everything we do at Boulder Crest is built on the idea of teaching and training men and women who are struggling to transform that struggle into strength and achieve posttraumatic growth in their lives.
MRC: Why do you think that message resonates so much with those you serve?
How things are isn’t how they have to be. It’s a philosophy and it’s a very practical and pragmatic focus that emanates from our founder, Ken Falke, and his prior work in training people in counter-IED work. In some respects, we’re training people to disarm the struggles that exist inside of us and to live great lives. In Ken’s language, we’re helping people to be as productive at home as they were on the battlefield. That’s based on the lineage of people who’ve served for thousands of years. It’s the idea that there are people in our society who possess wisdom about life that other folks don’t have and it’s incumbent on them to share it.
We have a quote in each of our gardens at Boulder Crest that says, ‘We must remember that one man (or woman) is much the same as another and that he (or she) is best who is trained in the severest school.’ And that’s what we believe.

People who are exposed to the stuff that the people we serve are exposed to, understand the fragility of life. They understand what matters. They understand the importance of being grateful. They understand the importance of relationships. Those are the true gifts of life that most of the rest of us don’t always fully understand.
MRC: How do you incorporate the concept of posttraumatic growth into your programs?
Posttraumatic growth is incorporated in a really explicit way in everything we do. Our flagship program at Boulder Crest is called Warrior PATHH (Progressive and Alternative Training for Helping Heroes) and that’s for members of the military and veteran community who are struggling, male and female. It’s a 90-day program that starts with seven days on the ground. It begins by introducing people to the notion of posttraumatic growth through a series of educational and experiential indoor/outdoor modules to teach them these ideas and allow them to put them into practice.
The goal is to make peace with their past, learn to live in the present, and plan for a great future, and to do that in a peer-based environment with fellow veterans and service members as well as instructors who are also veterans and first responders.
MRC: Warrior PATHH is one of your flagship programs, but you also have another exceptional program called Struggle Well. What can you share about that?
Struggle Well is all about how we bring those notions into the military world in a way that catalyzes people to think differently about themselves, their struggles, and their life in the hopes that they might not need a program like Warrior PATHH. There are two goals of Struggle Well: the first is to normalize struggle.
Struggle is a real part of life, it has an impact. When it has those impacts, it tends to feel like we’re the only person who’s ever been through it and that we’re irrevocably broken. The second is to democratize the ability for people to struggle well. This is all about giving people the skills, training, and practices that allow them to navigate the inevitable ups and downs of life in a healthy and constructive fashion.

MRC: How do you incorporate families and loved ones into your programming?
Boulder Crest partners with Songwritingwith:Soldiers on our Couples PATHH program, which is designed to bring Warrior PATHH graduates back with their spouses and loved ones, so they can have a shared experience. It’s super important to realize that struggle is contagious in a family. If you’re trying to lift one person up, you have to make sure you’re lifting up the entire family or else you probably won’t succeed.
Our original programming is Family Rest & Reconnection. At the heart of posttraumatic growth is the idea of trust and connection and giving families a chance to reconnect, rest, and recharge in a safe and peaceful setting, allowing them to foster or rebuild the trust and connection that’s the hallmark of any great relationship. It’s the fuel and foundation for growth to occur in people’s lives. There is programming for individuals, for couples, and for families.
MRC: As an organization, Mission Roll Call is committed to reframing the narrative around the stigma of post-traumatic stress disorder and prefers to use the term post-traumatic stress. Do you think posttraumatic growth is the next logical step in the conversation to help educate and demonstrate the hope that can follow trauma?
It’s interesting because a number of years ago, I was part of a leadership program and interviewed with one of President George W. Bush’s top staffers, and he said, ‘We thought we did a great job trying to drop the d (in disorder), and you did one better and added a ‘g.’ I do think this is the next part of that journey.
I think whether you drop the d or not, PTS and PTSD have a certain feeling and weight to them that often makes people feel like they’re destined to live diminished lives. And the thing that people lose in that situation is hope. If human beings don’t have hope, they lose agency and any sense that their actions will create change in their life. You can become nihilistic and quite cynical, jaded, and isolated. It leads to lots of bad outcomes from suicide to substance abuse issues.
To me, it’s not an either-or. It’s about balancing this conversation. It’s reminding people that symptoms are real but so is the possibility for growth. There’s a lady I deeply admire who lost her fiance who was a first responder in an ISIS-related shooting in 2015. Her name is Mandy Pifer. And she said, ‘You have to know posttraumatic growth exists for it to happen. You have to know it’s ok for good things to happen after really bad things.’
I think there’s an aspect of permission and awareness that people cannot reach for things that they cannot see. One of my favorite parts of our programs is when we start to talk about posttraumatic growth, and the most common response from veterans is, ‘Why has nobody told me this before? All I’ve ever been told is all the ways my life is going to be damaged or diminished because of what I’ve been through.’ And I think that in and of itself says everything about the importance of telling both sides of this story. It reminds people that all is not lost and that how things are isn’t how they have to be. Growth isn’t just a possibility, it’s potentially an inevitability.
Struggle, trauma, and difficulty are a part of all of our lives. We don’t want it and we don’t wish it on ourselves, but it still comes. It’s incumbent on us to realize it’s our choice what to do with it.
MRC: How can veterans, military members, first responders, and their families get involved with the Boulder Crest Foundation?
If you or someone you know is interested in participating in any of Boulder Crest’s programs, you can apply through our website, bouldercrest.org. We also offer opportunities for veterans and first responders to get involved as mentors and volunteers, helping to support their peers on the journey to posttraumatic growth.
For participants, the data in our programs is off the charts. People come in way above the clinical threshold for PTSD and they leave well below. They get to a place where those things don’t dominate their lives – and that’s in seven days. It doesn’t take long for people to realize, “Wow, I’ve been trapped in this prison, and the key to get out is in my pocket.’
MRC: Is there anything else you want to share about posttraumatic growth?
Trauma is often seen as insurmountable; a full stop in the story of our lives. But what if it can be a catalyst for forging a new path — one filled with passion, purpose, connection, growth, and service? That is posttraumatic growth.
For far too long we have focused exclusively on the negative impacts of trauma and struggle. The result is that we are left feeling permanently diminished and damaged; a victim to the worst experiences of our life. That must change. And that’s why we are starting a movement to Choose Growth.

Choose Growth shines a light on the opportunity to grow in the aftermath of trauma. Choose Growth changes the story around struggle and trauma and teaches the world to thrive post-trauma; moving the conversation from “PTSD” to “PTG.”
I would encourage anyone reading to watch this video and share it with your friends and family. The more we share, the more we grow. Connect with others and share the message of Posttraumatic Growth far and wide.
Watch: Choose Growth
Boulder Crest Foundation is at the forefront of transforming the lives of veterans, service members, first responders, and their loved ones through the power of PTG. By focusing on holistic and long-term healing, they offer a beacon of hope for those grappling with the challenges of struggle and trauma.
Join Mission Roll Call as we support Boulder Crest Foundation’s mission and help transform more lives. Visit this link to learn more and find out how you can get involved.