
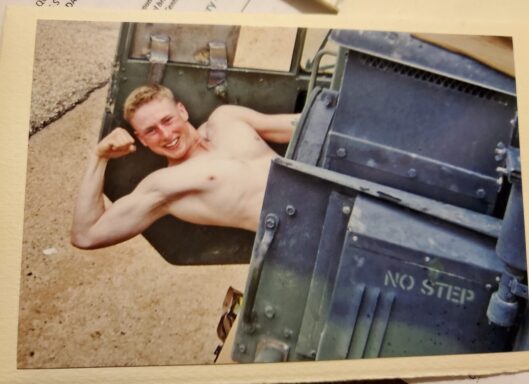
The desert was familiar long before Iraq. Owen grew up on a historic ranch in southeastern Arizona—rural, agricultural, hands in the dirt. Both grandfathers served, and from a young age, he knew he would, too. He enrolled in ROTC, then took his grandfather’s advice to “get your stripes before you lead men,” left college, and shipped to basic in 2003. By year’s end, he was in Iraq.
Owen became the lead gun-truck driver in and around Fallujah, a job he describes, without drama, as “the bomb magnet.” For most of that 13-month deployment, he rode in soft-skinned Humvees that the team reinforced with improvised steel. He survived multiple blasts. The worst came almost eleven months in, just after his unit received up-armored vehicles and rolled north from Kuwait, escorting a brand-new transport element.
He slid the armored window down to adjust a loose mirror bracket when an IED detonated ten meters in front of his truck.
“Post-blast, they said it was like three 155 shells daisy-chained,” Owen explained. “Within 50 meters is typically lethal. Somehow I’m still here.”
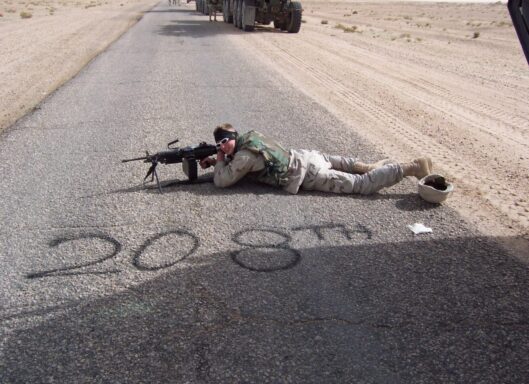
Shrapnel cored through metal: the gunner shield, antennas, tires. Owen was knocked unconscious yet somehow steered nearly a kilometer out of the kill zone before waking to a nine-line medevac call and smoke so dense he couldn’t see a hand in front of his face. The blast sucked the air from his lungs. Memory after that is splotchy—something he’s since learned is common with severe TBI. “When you don’t have memory, other people’s stories fill in the gaps,” he says.
Still, coming home was harder.
The VA moved him through polytrauma care and speech rehab. He pushed himself back into college to “work the brain like a muscle,” as he was advised. Courses that once came easy became a grind. He adjusted to the new normal he was told to expect, until, years later, symptoms surged: insomnia, driving and not remembering how he got there, word-finding problems, ocular migraines. The struggle spilled into his marriage. “It breaks your heart when your wife thinks you’re not listening,” he shared. “But sometimes I’d forget what she said ten seconds ago.”
Medications dulled the edges, added side effects, and didn’t solve the core issues. For Owen, the turning point came through an outpatient community-care program in Idaho, where he met a clinician named Sam who helped implement a protocol that paired neuroplasticity-priming, via closely supervised ketamine infusions, with a 40-dive course of Hyperbaric Oxygen Therapy (HBOT). The idea: increase the brain’s capacity to rewire, then supply oxygen-rich conditions to help it do the work.
It helped. A second 40-dive block followed at NorthStar Hyperbaric in Tucson under neurologist Dr. Carol Hendricks, whom Owen calls “an angel.” There, advanced DTI imaging helped target care. The plan included HBOT to “reset the hardware,” followed by neurofeedback to “reset the software.” For Owen’s specific injury profile, the team recommended additional dives and ongoing maintenance to guard against regression.
The progress was real, but the logistics were brutal. From Owen’s home, a single day meant two hours to the clinic, an hour in the chamber, four hours waiting between dives, a second dive, and two hours home. Nine hours, often while cognitively exhausted and on Arizona highways. It was unsustainable.
That’s when a fellow veteran mentioned a veteran service organization that might be able to help with an in-home system. Owen applied, was approved, and gained access to a home HBOT unit under physician guidance, making the protocol practical and safe for him to maintain.
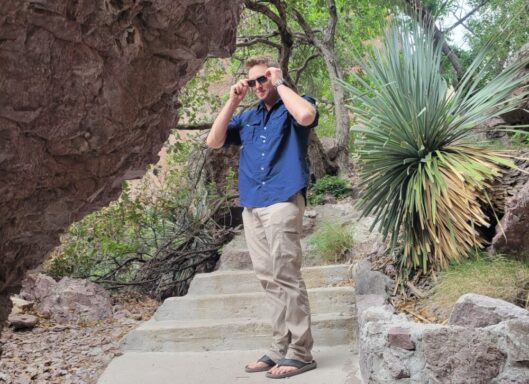
“HBOT has been a godsend. I care most about quality of life—being present for my wife and family. This gives me a chance at that,” Owen said.
HBOT wasn’t a magic wand, but it was a doorway. With brain-stem-related dysregulation after blast exposure (think vagus nerve and autonomic functions), Owen also manages complex downstream issues, including autoimmune complications. He’s already had two sinus surgeries, with a third scheduled, and coordinates care that may include stem-cell work and neuro-endocrine support.
Along the way, he’s become a student of brain healing—pointing other veterans to Dr. Norman Doidge’s The Brain’s Way of Healing and The Brain That Changes Itself, Dr. Dan Engle’s Concussion Repair Manual, and Dr. Kabran Chapek’s Concussion Rescue.
He’s become an advocate, too, because access remains the hardest part for many veterans.
Owen is frank about systemic hurdles he and his peers face: TRICARE policies that require numerous steps before considering certain modalities like TMS; VA/DoD pathways that still treat HBOT for TBI/PTS as outside the standard formulary; waiver processes many never reach. And he’s blunt about the stakes. “In the groups I’m in, it feels like every other week someone checks out,” he said. “It’s an epidemic. If we can reduce brain inflammation and restore function, we can save lives.”
Recently, Owen shared that Dr. Hendricks passed away—news that shook the HBOT community in Arizona and beyond. “She changed and saved so many lives,” he explained. He believes others will step up to carry the torch; in the meantime, his home unit and remote protocols keep his healing on track.
So what does better look like? For Owen, it’s simple: fewer barriers, more informed options, and coverage that meets veterans where they are: clinic-based or at home, as medically appropriate. “Heal the inflammation, and you can get your life back,” he said. “Heal the brain, and you save the person.”

At Mission Roll Call, we hear veterans like Owen loud and clear. Access and quality of care shouldn’t depend on a ZIP code, a waitlist, or a technicality. Veterans deserve evidence-informed options—including HBOT—without jumping through hoops that many won’t survive.
Stories like Owen’s highlight why Mission Roll Call continues to advocate for innovative treatments that meet veterans where they are.
Read our feature on how innovative treatments are making strides to support veterans—and why the system should be too.