Access to VA Healthcare
Is 64 days too long to wait for a specialist? That’s the average in some VA hospitals.
The VA provides quality healthcare. But many veterans struggle to access it.
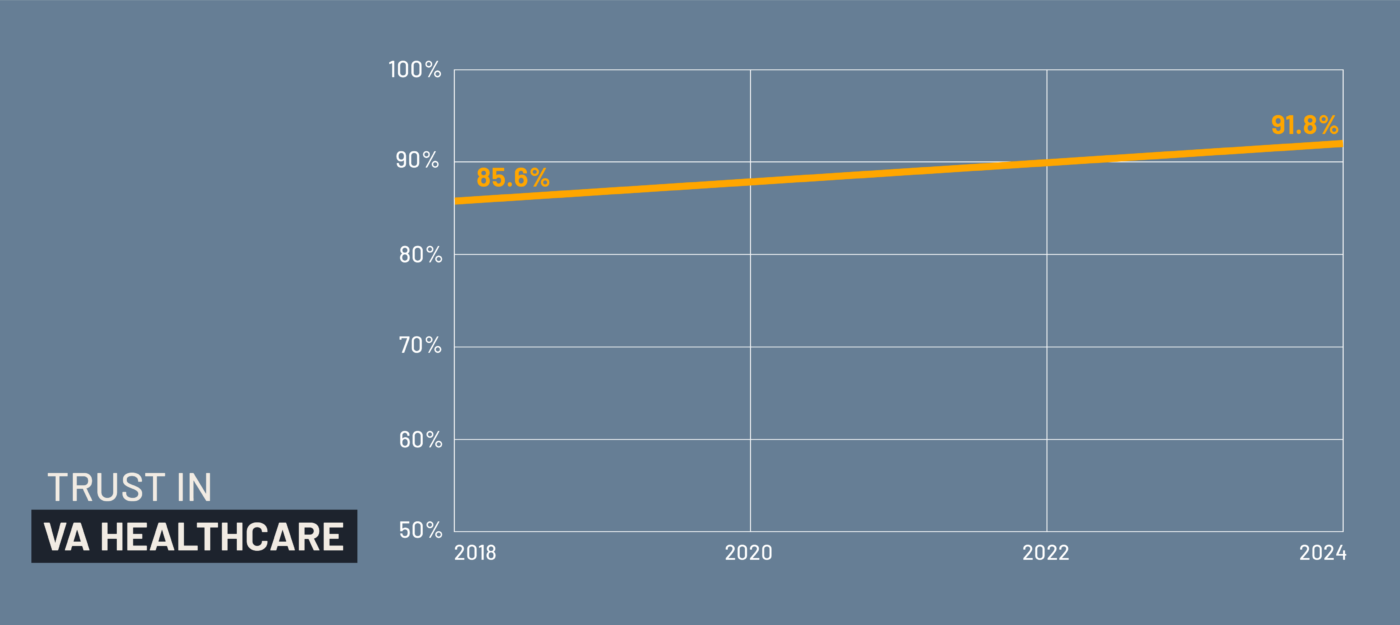
The good news? Contrary to popular belief, the quality of care provided through the VA’s healthcare system, the Veteran Health Administration (VHA), is not the problem. In fact, studies consistently find that Veteran healthcare is as good as, and often better than, civilian hospitals. VA hospitals are reported to have better survival rates for heart failure and stroke and better long-term outcomes for chronic conditions. And Veterans themselves typically report that they are satisfied with the care they receive – once they get it. Veteran trust in VA outpatient care has steadily increased, reaching 91.8% in April 2024, up from 85.6% in 2018.
Veteran Trust in VA Outpatient Care
The bad news: barriers to access prevent many veterans from ever experiencing that quality. Long wait times, lack of continuous care, distance from facilities and low enrollment rates remain the biggest challenges to the veteran community nationwide. These barriers not only reduce use of VHA services but also endanger the health and lives of those who have served.
Your generosity fuels meaningful change for veterans and their families. Every contribution allows us to connect, educate, inform and empower veterans in ways that will make a lasting impact on their lives now and the generations that follow.
Donate TodayThe Big Four Barriers
1. Wait Times: Delays undermine quality
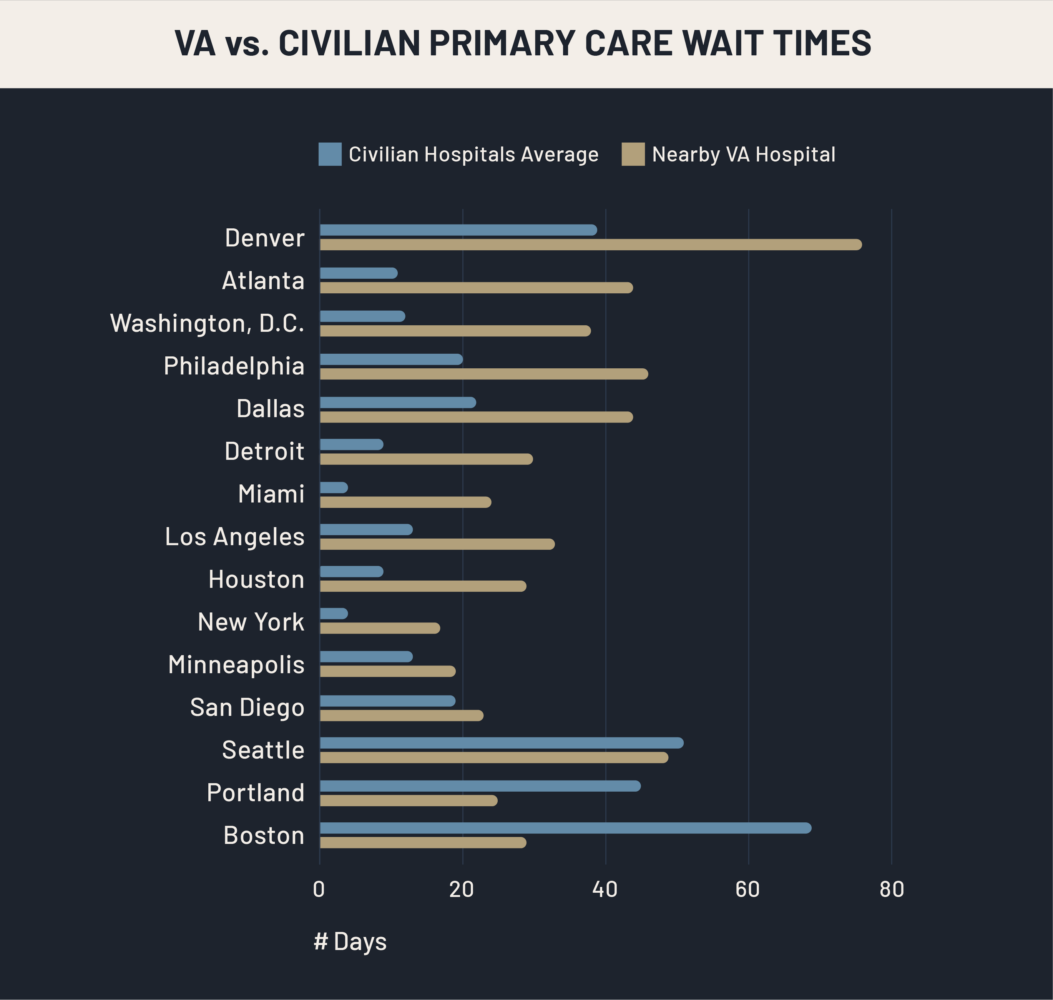
Long wait times remain the biggest challenge with VA healthcare. Notably, all Americans experience long wait times. Even though the industry standard for a non-urgent primary care appointment is 14 days, the average is typically much longer. A national study in 2024 reported an average of 38 days across the U.S.
For veterans, tracking data often show that VA wait times can be even longer than those in civilian healthcare – especially for specialty services. A comparison of wait times in 15 cities found that in 12 of them, veterans faced longer waits for primary care at VA facilities compared to nearby non-VA hospitals. In Atlanta, the wait time difference was more than a month – 44 days at the VA compared to just 11 at a civilian hospital. In Denver, the gap was even wider: 76 days at the VA versus 39 days at non-VA facilities. Houston, Miami, Los Angeles, Detroit, Washington D.C., and Philadelphia all had longer wait times at VA facilities by more than two weeks.
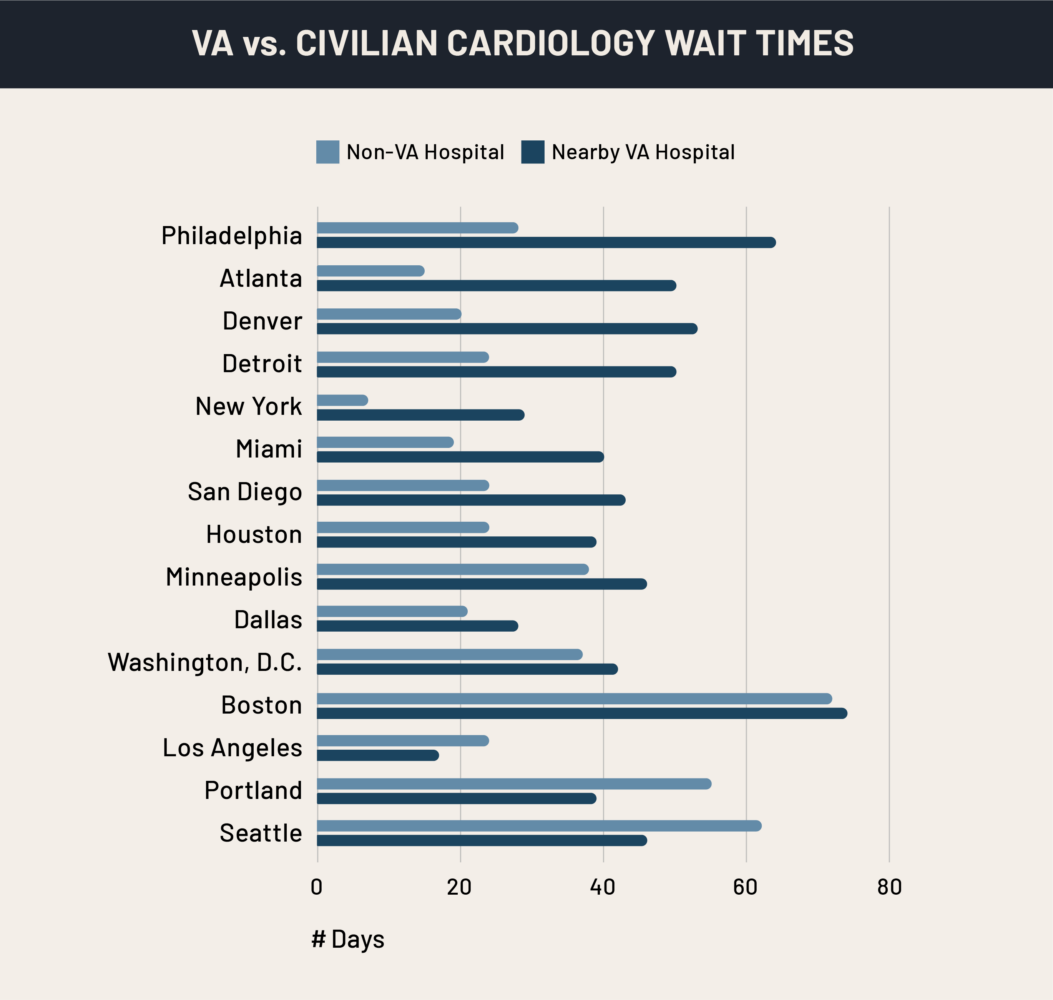
Wait times for specialists are similar and often worse. Veterans in Atlanta, Denver, and Philadelphia waited weeks longer than civilians to see a VA cardiologist. In Philadelphia, the average wait was 64 days at the VA compared to 28 days in the civilian system. For conditions where time is critical, like heart disease – a leading critical health risk – these delays can be more than frustrating. They can be dangerous.
That said, VA wait times are not always worse. In some areas, including Miami, Los Angeles, and New York, veterans were able to see providers more quickly at VA facilities than at nearby civilian hospitals. For a cardiologist visit, VA care was faster in Los Angeles, Portland, Seattle, and Washington, D.C. This means the problem is more about uneven access – where a veteran lives determines how long they wait and how quickly their condition is addressed.
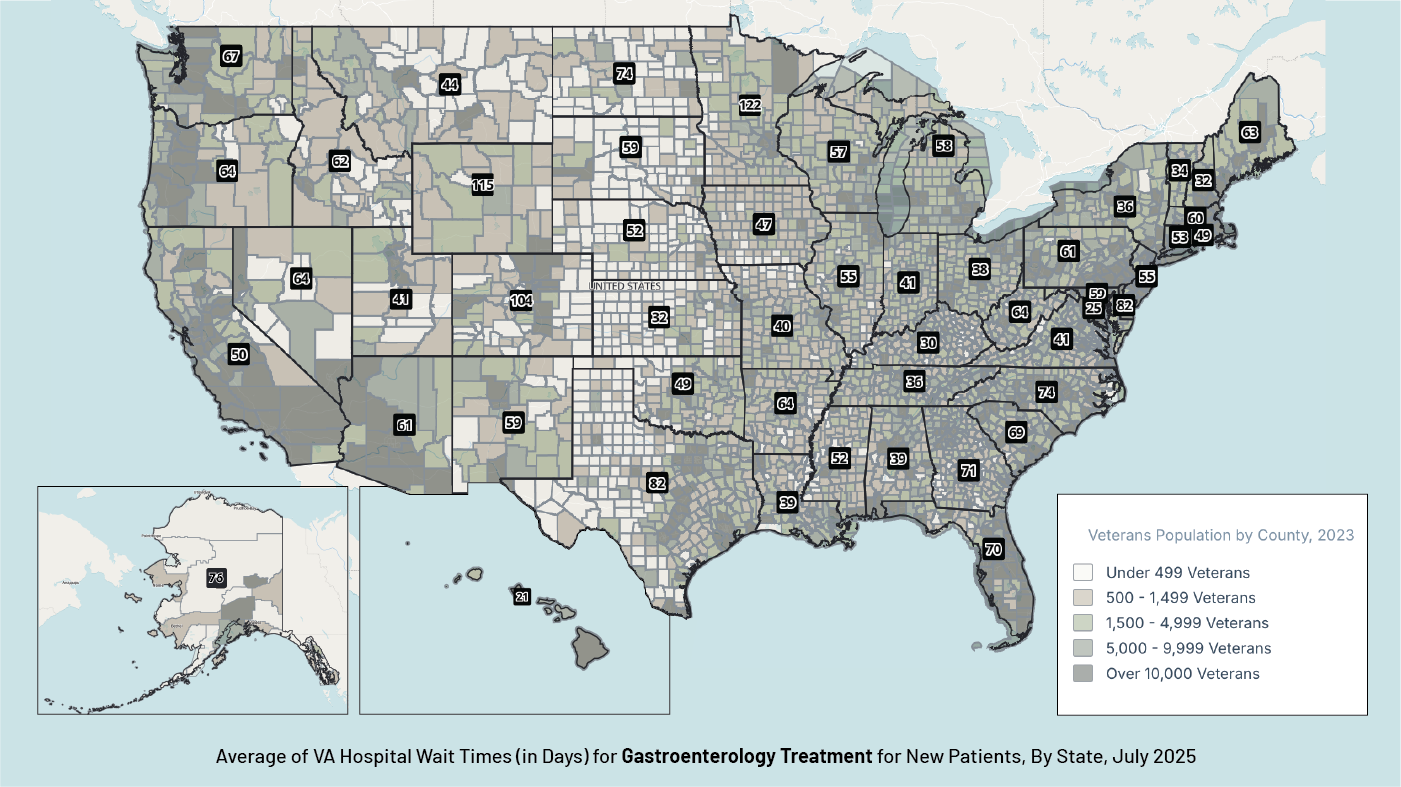
Other specialties experience even longer wait times. In July 2025, wait times for new patients with gastro-intestinal issues were significantly longer. A veteran would have to wait nearly three months for an appointment in Texas or Florida, while Minnesota, Wyoming, and Colorado experienced delays of more than 100 days.
# of Days for a New Gastroenterology Appointment at VA Hospitals
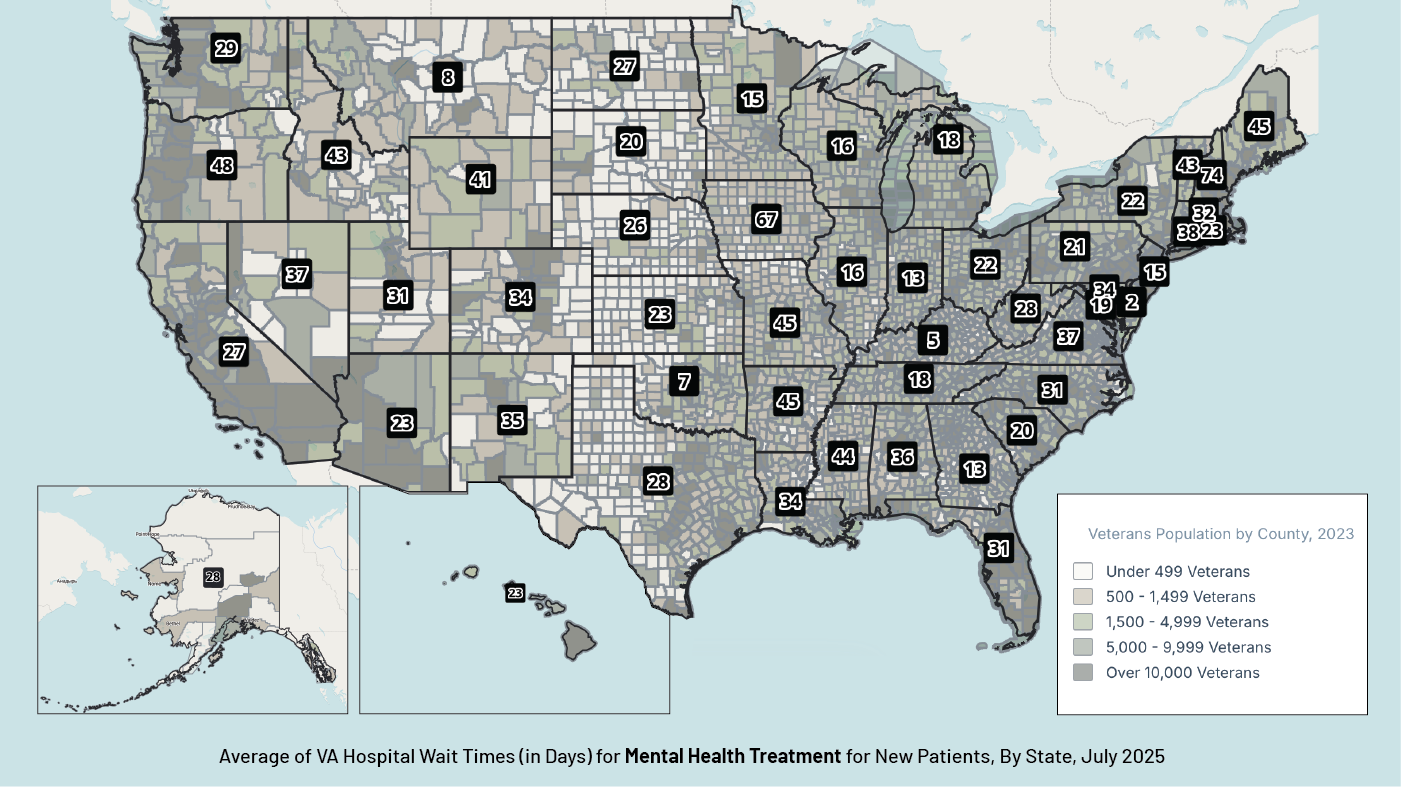
A high priority specialty for veterans is mental health care. When a veteran is experiencing the onset of a mental heath crisis, a delay can be life threatening. In the map below are new patient average wait times for a mental health appointment at VA hospitals, by state, from July 2025. For comparison, the population of veterans in each county is shaded to show higher and lower concentration of veterans. Long waits are especially common in states with more veterans – California, Texas, and Florida – where the average wait time is between 27 and 31 days for a new patient mental health appointment.
# of Days for a New Mental Health Appointment at VA Hospitals
Long wait times prompted recent initiatives to expand veteran access to healthcare through the private healthcare system, called community care programs. However, all healthcare faces wait-time challenges. Providing access to these hospitals under the 2018 MISSION Act gives veterans more options, but it isn’t a solution to the VHA access issue, nor does it solve the wait time problem.
Additionally, VA services provide specialized care that is informed by veterans’ unique experiences and care needs – something many civilian healthcare providers lack familiarity with.
2. Lack of Continuity of Care: Quality requires consistency
In addition to having to wait to see a doctor, veterans also experience “disjointed” health care, or a lack of continuity of care.
Veterans frequently find themselves retelling their medical history to new doctors because turnover is high among VA medical providers. This is especially harmful for veterans suffering from ongoing, complex and chronic health issues, since they need long-term support and consistent care. High turnover also prevents VA patients from building trust with their provider, which is a top reason veterans seek care outside of the VA. To quote just one veteran’s account: “At the VA, I’ve probably gone through 12 [primary care providers] in 2 years.” That inconsistency makes it challenging to build long-term provider-patient relationships that are essential to effective care.
In addition to the constant turnover of doctors, VA hospitals are more likely than civilian hospitals to serve as “teaching” facilities, where interns and residents rotate regularly. While this model supports medical education, it can add to veterans’ sense that their care is fragmented or inconsistent.
Continuity matters. Coordinated, stable care is especially important for veterans managing multiple health conditions or ongoing treatment. Without it, even a good individual visit falls short of meeting veterans’ long-term needs.
3. Geography: Distance puts care out of reach
More than 20% of veterans reside in rural areas. For these veterans, simply reaching care is often the greatest hurdle. VA facilities are not evenly distributed across the country, and in many rural locations, veterans may have to travel hours to reach the nearest medical center. For example, there is only one VA hospital in Maine, which means that some veterans travel an average of four hours to reach it. The commute could easily double in harsh winter weather conditions. That travel burden often makes it even harder, requiring taking time off from work for the visit, arranging childcare and securing reliable transportation. Limited public transportation options in many parts of the United States only make matters worse.
On top of the issue of distance, rural veterans are less likely to have reliable internet connectivity, making it hard to connect to the VA’s digital outreach and scheduling systems. Missed opportunities in outreach contribute to delayed access, especially for vulnerable groups like women veterans or those experiencing homelessness.
Adding to this, many rural communities struggle with high rates of substance abuse, poverty and homelessness, meaning veterans in these areas are particularly at risk and in need of access to care. Chronic illnesses such as hypertension and diabetes are common, along with service-related disabilities, such as PTS, hearing loss and burns or scars, and other mental health issues.
In the civilian healthcare space, rural hospital closures across the United States have made headlines, so this access issue is not unique to veterans. Rural veterans that may be using non-VA facilities through community care programs will feel the pinch even more. Without more consistent VA hospitals and clinics, the promise of high-quality care remains out of reach for millions of veterans.
4. Low Enrollment: Millions missing out
Among the 18 million current veterans, approximately 9 million have enrolled in the VHA, and only 6 million have used at least 1 benefit in the previous year. That means millions of veterans are potentially missing out on the high-quality, affordable healthcare that they’ve earned.
The reasons are complex. For many, the barrier begins with awareness. Veterans often don’t know they qualify: Over 40 percent report not knowing their VA healthcare benefits. Others discover the system only when they need care, at which point they face paperwork hurdles and delays at the exact moment when access care is most needed. Organizational and logistical barriers can play a major role in the lack of access to care.
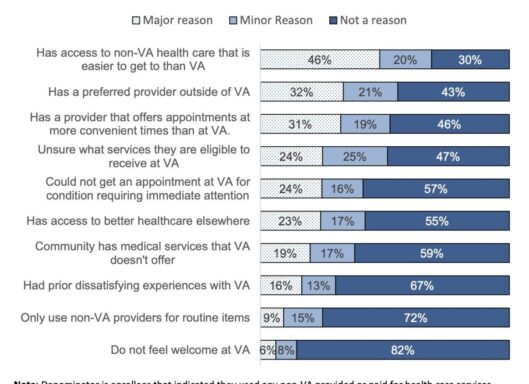
Even among those who are enrolled, many veterans choose not to use VA services. Convenience is the main reason: 47% of veterans reported using VA care for most of their needs, but nearly a quarter relied primarily on civilian providers. The most common reasons for using services other than the VA were easier access to appointments at non-VA facilities and a preference for existing, trusted providers outside the VA system.
Rural veterans again face unique challenges. Without consistent internet or mobile access, many never receive information about their benefits or available services. Outreach is critical: missed opportunities in communication leave veterans disconnected from a system that could serve them well. It is important to ensure that veterans are aware of what they qualify for, how to enroll and how to access care once they are enrolled.
The result is a paradox: the VA offers some of the best care available for conditions that disproportionately affect veterans, but millions either don’t know about it, can’t access it, or choose not to use it.
Conclusion
The Veterans Health Administration has proven it can deliver high-quality care – often better than what is available in the civilian system. But quality is not the problem. The real barriers lie in access: the distances rural veterans must travel, the long waits for appointments, inconsistent healthcare providers, and the millions who remain unenrolled or disconnected.
For veterans, these challenges shape whether they receive care at all, how quickly their conditions are treated, and whether they experience recovery or decline. Understanding these barriers is the first step toward ensuring that every veteran, no matter where they live or how connected they are, can access the quality healthcare they deserve.
Organizations That Can Help
Outreach is key. In our Resource Directory we list a variety of partner organizations who are ready to help. These include:
Avalon Action Alliance
Avalon Action Alliance specializes in providing life-changing treatment for veterans. Through Avalon’s Alliance Partnerships, a veteran can be matched with a specialized program that focuses on PTS, substance abuse, or traumatic brain injury.
Learn moreAmerica’s Warrior Partnership
America’s Warrior Partnership works with local communities and others to help support veterans and their mental health and prevent veteran suicide.
Learn moreWounded Warrior Project
Wounded Warrior Project is dedicated to supporting post-9/11 wounded, ill, or injured veterans and their families in all facets of life, including health care and mental health, including mental wellness and physical health wellness programs.
Learn moreMountain Valor
Mountain Valor focuses on connecting veterans in rural Virginia with the resources they deserve, from finding shelter to securing healthcare or transportation to resources.
Learn moreBoots to Health Foundation
Boots to Health Foundation helps veterans with physical health and wellness programs to help them live their best lives.
Learn moreThe VA
The VA offers resources for minority veterans, including benefits and direct loans for Native American veterans.
Learn more