As we recognize Post-Traumatic Stress Awareness Month, it’s essential to highlight the remarkable work of Mission Roll Call’s nonprofit coalition partners dedicated to supporting veterans and their families.
One impactful organization is the Avalon Action Alliance. Avalon is focused on changing how our healthcare system cares for those who have served. Through an alliance of partners, Avalon connects veterans with life-changing care and eliminates barriers to access, including geographical and financial obstacles.
Avalon’s comprehensive approach is vital in transforming lives. Trauma affects every aspect of an individual’s life, and each person’s experience is unique. Avalon’s integrated care model addresses the mind, body, and spirit; ensuring holistic healing while providing personalized support. Recognizing that trauma impacts the entire family unit, Avalon includes family members in the healing process. This inclusive approach strengthens family bonds and promotes collective well-being.
Avalon Action Alliance concentrates on four key areas to assist veterans and their families dealing with Traumatic Brain Injury, Post-traumatic Stress, and Substance Abuse:
- Brain Health Services: Avalon provides access to various brain health services through an alliance with seven TBI Medical Centers, 11 Posttraumatic Growth Programs, and two Substance Abuse Treatment Centers. These programs help individuals learn skills to overcome post-traumatic stress, substance abuse challenges, and persistent symptoms from traumatic brain injury.
- Physical Health and Wellness: Avalon believes there’s a direct link between physical and mental well-being and has developed programs to promote physical health, fitness, and nutritional counseling.
- Integrative Therapies: Avalon integrates various therapies, such as equine horse therapy, art therapy and mindfulness practices to provide unique ways for veterans to process their experiences and find healing.
- Community Building: Avalon’s alliance of partners fosters a sense of belonging and mutual support among veterans and their families. Veterans challenged with PTS-related symptoms are often isolated, and care is typically limited to symptom-suppressing medication. Avalon’s posttraumatic growth programs offer an alternative solution to life-long medication. Their care is based on the science of posttraumatic growth. Non-clinical training is provided by staff who have also served, creating long-term peer networks that veterans can leverage for sustained support.
Community connection is a priority. Building a supportive community helps veterans and their families feel understood and valued. Avalon’s community initiatives reduce isolation and create lasting connections. Avalon’s approach is changing lives and creating better days.
“Change doesn’t happen overnight,” said Mike, a U.S. Army veteran and Posttraumatic Growth Warrior PATHH participant. “I’m a work in progress. I’ve repaired my family, and I’m repairing myself. I don’t guarantee many things in life, but I can guarantee that Avalon’s posttraumatic growth program will change you.”
By raising awareness and supporting comprehensive care initiatives, we can contribute to the healing and recovery of veterans and their families. Avalon Action Alliance exemplifies the dedication and compassion needed to address the needs of our veteran community while making a tangible difference in the lives of those who have served.
As we honor Post-Traumatic Stress Awareness Month, let’s commit to supporting the invaluable work of Avalon Action Alliance and similar organizations. Together, we can ensure our veterans receive the care and resources they deserve.
If you or someone you know is a veteran (or first responder) in need of support for invisible wounds like Traumatic Brain Injury, Post-traumatic Stress, and Substance Abuse, please visit Avalon Action Alliance at www.avalonactionalliance.org to learn more about its care model.
What You Need To Know About Post-Traumatic Stress Awareness Month
June marks Post-Traumatic Stress Awareness Month, a crucial time to acknowledge the challenges faced by those who have experienced trauma and to advocate for their mental health and well-being. At Mission Roll Call, our commitment to supporting veterans and their families is unwavering, and this month serves as a poignant reminder of the invisible wounds that can be carried within our community.
Some, including Mission Roll Call, prefer using the term PTS instead of PTSD to reduce the stigma associated with the word “disorder” and to challenge the stereotype of “broken veterans.” Therefore, PTS will be used throughout the rest of this article (and in all MRC messaging) to promote a more understanding and supportive narrative.
Post-Traumatic Stress (PTS) vs. Post-Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress (PTS) affects millions of individuals, including veterans who have served our country with bravery and dedication. The transition from military to civilian life can often exacerbate these struggles, making it imperative that we come together to provide understanding, resources, and support.
PTS has often been conflated with Post-Traumatic Stress Disorder (PTSD), but it’s crucial to distinguish between the two. PTS is a natural and sometimes adaptive response to trauma, not a mental illness.
Many people, including civilians, experience PTS after extremely stressful events, such as sports accidents, falls, or more severe incidents like war or assaults. Unlike PTSD, PTS is not chronic, and individuals typically find relief in the short term.
In contrast, PTSD is a medically diagnosed condition requiring clinical treatment. Symptoms can be chronic, lasting a year or more, and necessitating ongoing medical attention. PTSD symptoms often appear within a month of the traumatic event and, while similar to those of PTS (such as flashbacks, nightmares, and a racing heart), are more intense and enduring.
While PTS is a psychological injury that can affect anyone who experiences trauma, veterans are more susceptible to developing PTS compared to non-veterans. The VA estimates that at least seven out of every 100 veterans will experience PTS at some point in their lives.
Combat experience, in particular, can heighten sensitivity to loud noises or bright lights, trigger insomnia and other sleep disturbances, and make everyday situations feel more stressful than before.
Moreover, veterans often encounter distinct barriers to accessing adequate mental health treatment. Research shows that less than half of veterans needing mental health services receive treatment, and among those who do seek help for PTS and major depression, less than one-third receive evidence-based care.
These statistics underscore the need for comprehensive mental health care that adopts a holistic approach to veterans’ needs.
Ways To Support Veterans and Their Families
In 2022, Mission Roll Call conducted an annual research survey on Americans’ attitudes toward veterans’ issues and found that 60% believe veterans experience post-traumatic stress (PTS) significantly more than their civilian counterparts.
Additionally, nearly half (46%) of U.S. adults think the federal government has been “not very effective” in handling veteran healthcare, including mental health support. This indicates a substantial opportunity for individuals to support our nation’s veterans, especially those dealing with PTS.
So what can we do to help? For starters, we can assist veterans in accessing helpful resources and information on healthcare benefits they may be eligible for. It’s a big reason why June is dedicated to PTS awareness.
If you know a veteran showing symptoms of PTS, consider the following actions:
- Educate Yourself: Learn about PTS and its effects. Understanding the condition can help you better support your loved one or friend.
- Encourage Professional Help: Suggest they speak to healthcare providers who specialize in veterans’ needs and help them find a therapist if recommended.
- Engage in Physical Activities: Participate in physical activities with them. Consistent exercise, like jogging, walking, or biking, can improve mental health.
- Offer Support: Provide a listening ear and let them know you are there if they need to talk about their experiences.
- Connect with Peers: Help them connect with other veterans in similar situations through online forums, Facebook groups, or nonprofit organizations having an impact in the space.
Later this month, MRC will share more details about one of those organizations that may be able to help, a nonprofit called Boulder Crest Foundation.
At the heart of Boulder Crest’s mission is the Warrior PATHH (Progressive and Alternative Training for Healing Heroes) program. This program is designed to transform the way veterans and first responders think about and respond to their traumatic experiences. Instead of viewing PTS as a disorder, Boulder Crest promotes the concept of Post-Traumatic Growth (PTG), helping individuals harness their trauma as a catalyst for personal development and resilience.
Boulder Crest Foundation Warrior PATHH participants
Supporting veterans and their families as they navigate the challenges of post-traumatic stress (PTS) is a collective responsibility that requires empathy, awareness, and action.
Education is the foundation of effective support. By learning about PTS and the available resources, we can better assist veterans in accessing the care they need. Practical help, such as guiding them through healthcare systems and connecting them with veteran-focused organizations, can alleviate some of the logistical burdens they may face.
Emotional support is equally crucial. Being there to listen, encouraging open communication, and offering reassurance can make a significant difference in a veteran’s journey toward recovery. Building strong, supportive relationships and fostering a sense of community can mitigate feelings of isolation and promote mental well-being.
Advocacy and awareness are powerful tools in the fight against the stigma surrounding PTS. By raising awareness, advocating for better services, and volunteering with veteran-serving organizations, we can contribute to systemic changes that benefit veterans and their families.
Ultimately, creating a supportive environment where veterans feel understood and valued is essential. Encouraging self-care, respecting their boundaries, and involving their families in the healing process can lead to more comprehensive and sustained recovery.
Join us this June as we amplify the voices of those impacted by PTS, share their stories, and highlight the resources available to aid in their recovery. Together, we can foster a community of compassion and resilience, honoring the sacrifices made by our veterans and their families and ensuring they receive the care they deserve.
Are you a member of the Mission Roll Call community? If not, please subscribe and join our polls to let your voice be heard, and follow us on Facebook, Instagram, and LinkedIn for the latest news and updates.
Memorial Day is a solemn occasion to remember and honor those who have made the ultimate sacrifice in service to our country. It is a day to collectively acknowledge and honor the bravery and dedication of those who have given their lives in military service, and to reflect on the enduring impact of loss on families and communities.
The Gold Star family is one that has experienced a loss of a loved one – an immediate family member – who died as the result of active-duty military service. Those who die in service to their country leave behind parents, siblings, spouses, children and extended families. These are recognized as Gold Star families. The title is meant to honor the service member’s ultimate sacrifice while acknowledging their family’s loss, grief, and continued healing.
For families of fallen heroes, those feelings can be heightened during Memorial Day commemorations.

Memorial Day can be a deeply emotional time for veterans, too, bringing feelings of grief and sorrow to the forefront. Veterans often develop strong bonds with their fellow service members, forged through shared experiences and hardships. Memorial Day serves as a stark reminder of these losses, and the memories of friends and colleagues who did not return home can evoke a deep sense of grief. For some veterans, the day may amplify feelings of isolation and loneliness, particularly if they feel disconnected from the civilian population who may not fully understand the depth of their experiences and losses.
While the pain of losing a loved one can be overwhelming, there are many organizations dedicated to supporting veterans, families, and individuals as they navigate their grief. Here, we highlight five outstanding organizations that provide essential resources and support for those coping with loss on Memorial Day and beyond.

Boot Campaign
Boot Campaign is dedicated to igniting the inner patriot in all Americans and providing life-improving programs for veterans and military families. By raising awareness of the challenges service members face and offering holistic and personalized care, Boot Campaign supports veterans and families in their healing journey.
Their programs address the physical and emotional health of those left behind, ensuring that the memory of the fallen is honored through action and support.
Children of Fallen Patriots
Children of Fallen Patriots is committed to providing college scholarships and educational counseling to military children who have lost a parent in the line of duty.
The organization serves the families of servicemembers from all branches of the armed forces who have died as a result of combat casualties, military training accidents, service-related illnesses, suicide, as well as other duty-related deaths as ruled by the Department of Veterans Affairs.

Recognizing that the loss of a parent can create financial and emotional strain, Children of Fallen Patriots offers critical support to help these children pursue their dreams. Remembering the fallen also means supporting their children, ensuring they have the resources to succeed and honor their parents’ legacy. The vision of the Children of Fallen Patriots Foundation is to ensure that every child of a fallen patriot receives all necessary college funding.

Gary Sinise Foundation
The Gary Sinise Foundation serves our nation by honoring our defenders, veterans, first responders, their families, and those in need. They do this by creating and supporting unique programs designed to entertain, educate, inspire, strengthen, and build communities, including the Snowball Express and H.O.P.E.
Snowball Express serves the children of fallen military heroes, surviving spouses, and Gold Star families. Through community events, educational programs, and a special annual holiday retreat, Snowball Express brings together families to form lasting friendships and find comfort in shared experiences.
The holidays can be especially challenging for grieving families. Each December, the Gary Sinise Foundation hosts a five-day experience at the Walt Disney World Resort for 1,750+ children of the fallen and the surviving spouse/guardian.
The Gary Sinise Foundation Snowball Express
With special time to honor their fallen and a blend of fun entertainment and inspiring programs, these families can lean on their peers for support. These gatherings help families to heal, remember, and celebrate the lives of their loved ones in a supportive environment.
The Gary Sinise Foundation also offers broad support to veterans and others who have experienced trauma or loss. Its H.O.P.E. initiative – heal, overcome, persevere, and excel – seeks to bring people together to form a network of support. By sharing their experiences and reminding one another they are not alone, these groups can find joy in the present once again.

Folds of Honor
Folds of Honor provides educational scholarships to the spouses and children of America’s fallen and disabled service members, awarding over 52,000 educational scholarships since 2007. By alleviating the financial burden of education, Folds of Honor ensures that the dreams of those who have sacrificed so much are kept alive through the achievements of their loved ones.
Folds of Honor stands behind the symbol of a folded flag, as it reflects their mission to honor the sacrifice of America’s heroes while giving hope to the bearers of their legacy. This Memorial Day and beyond, Folds of Honor reminds us that honoring our heroes means supporting their families’ futures.

America’s Gold Star Families
America’s Gold Star Families offers support and services to families who have lost a loved one in military service. Their programs include peer support, grief resources, and memorial events that help families connect and heal.
Many people are unaware of the significance of the Gold Star banner and its meaning. America’s Gold Star Families is committed to educating others on this important designation, how to properly respond when meeting someone who has lost a loved one in service to our country and advocating for their needs.
By creating a community of support, America’s Gold Star Families ensures that no family has to grieve alone and that the sacrifices of their loved ones are never forgotten.
America’s Warrior Partnership
America’s Warrior Partnership aims to empower communities to support veterans and their families, including those who have lost a loved one in service. Their holistic approach focuses on proactive outreach and connecting families with the resources they need to thrive.
America’s Warrior Partnership empowers communities to empower veterans.
America’s Warrior Partnership Network is a national coordination platform that expands the reach of local veteran organizations by connecting them to national resources. When a local resource is unavailable or exhausted, veteran service organizations can work with AWP’s network to find vetted, quality partners to collaborate with in delivering needed services.
Individual veterans may also refer themselves to The Network when they are not sure where to go for a particular resource. By fostering strong community networks, America’s Warrior Partnership helps ensure that grieving families receive comprehensive support, honoring the legacy of their fallen heroes.

These organizations offer crucial opportunities for fellowship and community, helping veterans and families navigate the complex emotions that surface as they remember their fallen heroes. Grief is a deeply personal experience, yet it is often easier to manage when shared with others. Whether through virtual gatherings or in-person events, coming together to share stories and participate in traditions can provide solace and support.
This Memorial Day, as we reflect on the sacrifices made by our brave service members, let us also acknowledge and support the families and fellow service members who continue to bear the weight of their loss. By engaging with and supporting organizations like Boot Campaign, Children of Fallen Patriots, Gary Sinise Foundation, Folds of Honor, America’s Gold Star Families, and America’s Warrior Partnership, we can help ensure that the legacies of our fallen heroes are honored and remembered in meaningful ways.
Military Appreciation Month is a time to honor the service and sacrifice of our nation’s heroes. Their unwavering dedication to protecting our freedoms deserves not only our gratitude but also comprehensive support and resources.
This month, we want to pause and acknowledge some of the Veteran Service Organizations (VSOs) across the country that are committed to ensuring veterans and their families have access to the tools, programs, and communities that honor their service and empower them to thrive beyond their military careers.
At Mission Roll Call (MRC), our aim is to give every veteran and their loved ones a voice on the issues that matter most to them. We gather your opinions and feedback to understand and represent veteran priorities in our advocacy efforts each year, including veteran suicide prevention, healthcare and benefits, transition into employment, and veteran homelessness.
Fortunately, there are many reputable and committed VSOs creating an impact in the areas you’ve helped MRC identify as top priorities and beyond, and we’ve selected a few to share with you. We’ll continue to identify and distribute resources and information like this throughout the year, so please continue to check back for more.
Here are five veteran non-profits to know about:

Boulder Crest Foundation
The Boulder Crest Foundation focuses on post-traumatic growth, offering programs and retreats designed to help veterans and their families build resilience and thrive in their civilian lives.
They offer programs such as Warrior PATHH (Progressive and Alternative Training for Healing Heroes), a non-clinical path to post-traumatic growth; PATHH Discovery, a five-day retreat focusing on wellness and resilience; family programs, and online resources.
“It’s time to change the conversation from post-traumatic stress to post-traumatic growth,” said Josh Goldberg, CEO of the Boulder Crest Foundation.
Their programs incorporate elements such as wellness, mindfulness, and peer support, providing a holistic approach to mental health and well-being.

Team Red, White and Blue (Team RWB)
Team RWB’s mission is to enrich the lives of America’s veterans by connecting them to their community through physical and social activity.
In the military, service members push the limits of their well-being to support the mission. That selfless service posture has always been necessary because service members of every era knew they might be called to war. As they move into civilian life, many veterans carry that mission-first mindset with them, neglecting their health in the process.
Team RWB believes that veterans are America’s most resilient citizens — and it’s time for more veterans to prioritize their well-being first.
They organize a wide range of events, from fitness activities like running and yoga to social gatherings and volunteer opportunities. By fostering connections and promoting physical health, Team RWB helps veterans maintain a sense of purpose and camaraderie.

Team Rubicon
Team Rubicon unites the skills and experiences of military veterans with first responders to rapidly deploy emergency response teams in crisis situations.
Whether it’s natural disasters, humanitarian crises, or community service projects, Team Rubicon provides veterans with meaningful opportunities to continue their service while making a tangible impact on communities in need. In 2022 alone, 48,000 volunteers served 23,575 people across 140 communities through response and recovery operations, special projects, and skills training.
Team Rubicon’s vision is to support humanity and build resiliency for vulnerable communities across the world.

Avalon Action Alliance
Can you imagine what it must feel like to lose parts of yourself to invisible wounds like Traumatic Brain Injury (TBI), Post-Traumatic Stress (PTS), and Substance Abuse (SA)? Can you imagine how difficult it must be to integrate into civilian life when you feel lost and hopeless? This is the reality for some veterans and first responders.
Together, with an alliance of partners, Avalon Action Alliance connects our nation’s heroes with life-changing care.
Through advocacy, education, and support programs, Avalon addresses the unique challenges faced by military families, offering resources to enhance their quality of life and strengthen family bonds, including mental health, financial stability, and community integration.
Avalon Action Alliance’s focus on family support acknowledges that the challenges faced by veterans often extend to their families, and by addressing these challenges, they contribute to the overall well-being of the veteran community.

The Mission Continues
“Our vision is for all veterans with a desire to continue their service to be part of a movement to transform communities.”
The Mission Continues empowers veterans to continue their service by mobilizing them for volunteer work in select communities across the United States. Through service projects focused on areas such as education, homelessness, and neighborhood revitalization, veterans not only give back but also find purpose and connection as they work alongside fellow service-minded individuals.
To date, 93,600 volunteers have been activated in service to others, completing more than 8,600 service projects.
These organizations collectively represent a spectrum of support and opportunities for veterans and military families, addressing various aspects of their lives ranging from mental health and wellness to community integration, disaster response, family support, and continued service.
Through their innovative programs, dedicated staff, and collaboration with the veteran community, they continue to make a meaningful impact and enhance the lives of those who have served and their families.
When the Promise to Address Comprehensive Toxics Act (better known as the PACT Act) became law in August 2022, it increased benefits for veterans who were exposed to burn pits, herbicides, Agent Orange and other toxic substances during their military service.
The number of claims submitted has risen dramatically since the PACT Act was passed.
According to the VA, in 2023, veterans submitted a record 2.4 million claims – 39 percent more than in 2022 – and the VA delivered a record $163 billion in earned benefits to more than 1.5 million veterans and survivors.

If you’re not sure if you’re eligible for disability claims, find out more here.
Veterans have multiple options for filing claims:
- Filing their claim with the VA themselves, without assistance
- Using the services of a nonprofit VSO, like the VFW
- Hiring an attorney or other for-profit entity
You are not required to use any assistance in filing your claim.

How to get started
If you are receiving help in filing your claim through a VSO, an agent or an attorney, you will need to sign over a Power of Attorney, allowing the organization or individual to access all medical and military records in order to act on your behalf. This Power of Attorney is limited only to VA claims. Without it, the VSO or attorney will not be able to receive any information about the claim. Veterans who do not wish to sign over a Power of Attorney should consider filing their claim independently.
These VA videos help explain the process:
What are the benefits of filing your disability claim with the help of a VSO representative?
The majority of VSOs were started by veterans for veterans. They understand the process and are up to date with current legislation affecting veterans. VSOs do not charge for these services.
A representative from the VSO will help you step by step through the process and can tell you if you need any supporting documents or any additional forms. Once your claim is filed, they will track the claim through the VA system and act as the liaison between you and the VA, explaining the outcome to you.
The following organizations are accredited by the VA and provide services free of charge. You do not have to be a member of these organizations to use their services:
- Veterans of Foreign Wars
- Amvets
- Vietnam Veterans of America
- Disabled American Veterans
- Paralyzed Veterans of America
- The American Legion
- Iraq Afghanistan Veterans of America
- The Wounded Warrior Project

What are the benefits of filing your disability claim with the help of a for-profit entity?
Some for-profit, independent claims agents and attorneys are VA-accredited. Being accredited by the VA means that the individual or company has undergone a character review and passed an examination about VA law.
For-profit entities charge for their services. VA-accredited for-profit entities, such as claims agents and attorneys, may be able to help you if your claim is denied, or not rated highly enough for your liking, and you want to submit an appeal (Note: VSOs can also help you with appeals). They may have more experience in handling these specific situations and can offer more personalized attention. VA Board of Appeals data show that in 2021, attorneys were more successful during appeals than agents or VSOs.
Some veterans choose to use one of these services when they have tried using a VSO in the past but weren’t happy with the result.
What is a “claims shark?”
Many companies who pitch their services to veterans offer relatively reasonable fees and are transparent about how these fees are structured. Unfortunately, alongside most VA-accredited or unaccredited for-profit entities (who provide genuine support at a reasonable fee), there’s also a lurking threat: claims sharks.
Claims sharks are individuals or companies, without VA accreditation, who exploit veterans by charging exorbitant fees to advise veterans on filing claims. These claims sharks take advantage of veterans, with predatory practices like burying fees in complex legal contracts.
In March 2024, several national veterans’ groups, including VFW, Wounded Warrior Project, Paralyzed Veterans of America and Blue Star Families, testified about claims sharks at a joint hearing of the Senate and House Veterans’ Affairs committees. According to the American Legion, “Unaccredited claims companies target veterans with fees as high as 600% of any future increase in their monthly VA benefits … leaving [veterans] with minimal compensation after legal fees are applied.”
In one lawsuit, a Maryland consultancy is accused of charging an Air Force veteran a fee of five times the increase in his monthly disability benefits. In another, an Army veteran experiencing PTS claims a North Carolina firm used deceptive practices and charged her five times her monthly benefits increase as well.
Because of the risk of excessive fees, U.S. Department of Veterans Affairs Secretary Denis McDonough advises veterans not to use for-profit services and to go to free, accredited VA partners instead.
Veterans’ reviews of for-profit entities are mixed. In a 2024 MRC poll, 2 in 3 veterans who said they had paid for support with their disability claim said they were happy with the service they received. In comparison, 4 in 5 veterans who used a free service said they were happy with that service.


How do you spot a claims shark?
Weeding out claims sharks from legitimate service providers can be complicated. The first thing to do is to verify if a lawyer or agent is accredited by the VA by searching the VA accreditation index.
Claims sharks typically target veterans through aggressive ad campaigns, especially social media ads. They may engage in the following fraudulent or unethical practices:
- Guarantee an increased disability rating or percentage increase
- Advertise expedited VA claims decisions
- Request login credentials to a veteran’s personal VA information
- Advise veterans to forego VA medical exams and refer veterans to their own network of doctors instead.
In addition, the law prevents lawyers from charging for assistance in filing an initial claim for VA disability benefits. A lawyer can only charge for assistance in an appeal. If an attorney is advertising their service for an initial claim, be wary.
How is Congress protecting veterans from claims sharks?
Congress is considering two pieces of legislation to protect veterans from claims sharks.
By law, individuals and companies can’t assist veterans in preparing their claims for disability benefits without accreditation from the VA Office of General Counsel, and they also can’t charge for those initial claims. But according to the VFW, the existing law is not enforceable, because it lacks criminal penalties.
The first piece of legislation, the Governing Unaccredited Representatives Defrauding VA Benefits Act (the GUARD VA Benefits Act) would make it punishable by law to solicit or receive payment for preparing a veteran’s disability claim. The bill, sponsored by U.S. Senator Jon Tester (Chairman of the Senate Veterans’ Affairs Committee), has strong support from veterans’ organizations like the VFW.
The PLUS Act for Veterans, on the other hand, is more measured than the GUARD Act. It would allow for-profit entities to assist veterans, but would require them to receive VA accreditation first. It would only be a criminal act to continue serving veterans without this accreditation.
Supporters of the PLUS Act say veterans should continue to have options when it comes to claims. Many veterans are okay with paying a fee for these services and should not be limited by law to only using not-for-profit organizations.
Takeaways: What to consider when using for-profit entities
- You can file claims free of charge using VSO organizations like American Legion, Veterans of Foreign Wars, Amvets, and more. You do not need to be a member.
- While for-profit entities do charge fees, many are transparent and want to provide a legitimate service. Pay attention to the fee structure to avoid predatory practices.
- Verify any claim agents and attorneys through the VA’s accreditation portal.
In conclusion, you can file your disability claim directly with the VA yourself, or you can use the services of an outside entity, like a VSO (for free) or a for-profit entity (for a fee). Each choice has advantages and disadvantages.
Most importantly, make sure you protect yourself: never pay for a service without being entirely sure what you are being charged and what you are receiving in return.
Observed annually on November 11, Veterans Day is a day for Americans to honor those who have served in the U.S. military. This Veterans Day, Americans should reflect on the debt we owe our veterans who have protected our way of life, and recommit ourselves to ensuring their success in post-military life.
There are currently more than 16 million living veterans in the United States. Yet despite two decades of conflict in the Global War on Terror, a recent Mission Roll Call national poll found that 67% of Gen Z does not know a veteran. And in a 2022 Mission Roll Call poll, we asked veterans, “After the United States’ exit from Afghanistan, do you think veteran issues have become less of a priority for the American public?” 75% said yes.
There are many ways to show veterans that you value their service, even if you don’t know a veteran. In this article, we’ll recommend some of the best ways to thank veterans based on data from real veterans. But first, we’ll discuss whether or not you should even thank a veteran for their service. Does it really matter?
Should you say “Thank you for your service”?
A few studies show younger veterans are uncomfortable with it and some civilians worry the phrase feels overused to the point of lacking meaning. Overall, however, veterans have told Mission Roll Call they really do appreciate it.
In 2023, Mission Roll Call asked veterans, “Does telling a veteran ’thank you for your service’ feel like an obligation, or genuine recognition?” 85% said it felt like genuine recognition.
But to make sure the phrase sounds sincere, follow it up with a question. Listening can be a powerful form of gratitude. A 2019 poll found that veterans actually prefer questions about their service to thanks. Ask how long they served. What was their job? What unit were they in? Most veterans are proud of their service and appreciate people showing genuine interest. That being said, be careful not to ask questions that are too probing and recognize that while some veterans want to talk about their service, others don’t.
One great way to “listen” is to watch Mission Roll Call’s “Veteran Voices” videos. In this series, we share the stories of veterans on topics like transitioning out of the military, starting small businesses, their experiences with the VA, and more.
Encourage the veterans you know to share their stories with Mission Roll Call. We believe in the power of veterans’ stories to inspire change, and the more veterans who share their stories publicly, the more others will know they aren’t alone.
What if you don’t know a veteran?
If you don’t know a veteran but want to say thank you, organizations like A Million Thanks and Soldiers Angels will help you send notes of gratitude to veterans. Engage your family and friends, school, church or business to write as well. These notes really do make a difference to veterans.
Another way, even if you don’t know a veteran directly, is to share messages of gratitude on social media. These can have an impactful reach outside of your immediate circle of contacts.
The fact is, there are also many other ways that you can thank, support and advocate for the veterans around you. Here are a few of the many ways that you can, practically, thank veterans for their service:
1. Recognize their continued service in your community
The values and habits the military instills from day one don’t disappear when veterans transition out. Coupled with the GI Bill, VA home loan, and numerous other benefits, the work ethic, discipline, and confidence the military imparts can rocket young men and women into successful careers or job tracks.
As we honor our country’s veterans this year, we should remember that their service continues long after they take off the uniform. While it’s important to focus on veterans in need, we can’t forget the many major contributions veterans continue to make to their community after they leave active duty. This year, thank a veteran by also thanking them for the service they’re doing after the military.
There are 9 million veterans in the U.S. workforce today. Values of selflessness, duty and integrity naturally lend to leadership positions and roles in business, public service, healthcare, law enforcement and national security. According to the most recent statistics, veterans represent 1 in 4 police officers, 1 in 5 firefighters, and 1 in 10 EMTs. And according to the U.S. Office of Personnel Management, approximately 1 in 4 current Federal employees is a veteran, with more than half a million veterans employed today in U.S. agencies around the world. Some studies have found that 10% of Fortune 500 CEOs have military service in their background.

Outside of their day jobs, veterans unselfishly continue to volunteer their time and money to their communities. In 2020-2021 – at the height of the pandemic – veterans averaged more volunteer hours per year than their civilian peers. Even outside of military and veteran-focused organizations, veterans can be seen volunteering to aid disaster relief efforts, in youth mentorship and other community programs.
One way for businesses to thank these veterans is to hire them. Veterans make excellent employees. They understand teamwork, are goal-oriented, have proven leadership skills, and are used to performing under pressure.
In a Mission Roll Call poll, 97% of Americans said they believe veterans make good employees. The Society of Human Resources Management (SHRM) reports that 68% of employers say veterans perform “better than” or “much better than” their civilian peers, and 63% say veterans are more resilient remote workers, compared to civilians. A LinkedIn study found that veterans also have lower turnover, remaining with the companies that initially employ them 8.3% longer than nonveterans.

For businesses looking to hire, the U.S. Department of Labor’s website features insightful resources and tips for attracting and hiring veteran candidates.
2. Support veteran-owned small businesses
9.1% of U.S. small businesses are veteran-owned, generating $1 trillion in annual receipts and employing more than 5 million Americans. As we approach the holidays, make an effort to support veteran small businesses, both local and online.

A Small Business Administration study found that veterans are 45% more likely to be self-employed than nonveterans. And because veterans are more likely to hire other veterans, when you shop at a veteran-owned small business, chances are you’re also supporting veteran employees.
You can find veteran-owned shops and services near you in directories like American Veteran Owned Business Association and Buy Veteran. You can also search for veteran-owned businesses by state to find the ones in your area.
3. Volunteer to help veterans
If you know of a veteran in your neighborhood, offer to mow their lawn, help with yard work, or deliver a meal. Even if they don’t “need” the help, the gesture is meaningful.
There are also thousands of organizations and nonprofits aimed at helping veterans. Consider making a monetary donation or volunteering your time or skills, but make sure you do your research first. In the past, Mission Roll Call has highlighted the work of America’s Warrior Partnership, Boulder Crest Foundation, Camp Southern Ground, and Black Ops Rescue, among many others. You can also find volunteer opportunities in your area at the VA Voluntary Service Office, including driving/escorting veterans to their medical appointments.
The ETS Sponsorship Program provides Military Transition Support to service members who are returning to civilian life. The program, in partnership with the VA, matches a transitioning service member with a sponsor within their new post-military community. Visit their website to be matched with a transitioning service member. Sponsors share their knowledge of the local area and available resources, and serve as a touchpoint for veterans, through a weekly “check-in” call or text and a monthly in-person meeting.
Another way to show gratitude to veterans is to sponsor a service dog. Service dogs are life saving heroes for the veteran community, providing essential support and companionship. There are several organizations that allow you to sponsor a companion or service dog for veterans. K9s for Warriors, Patriot PAWS, Semper K9, Warrior Canine Connection, and Labs for Liberty are among those we recommend. Watch the “Veteran Voices” video of how a service dog became a lifeline for U.S. Army Combat Veteran Greg Stevens.
4. Advocate for veterans
On Veterans Day, don’t just say “thanks” and wait for someone else to do the rest. Join Mission Roll Call to advocate for veterans on Capitol Hill.
Our country and our government still have a long way to go supporting veterans. Mission Roll Call’s 2023 research study found that 42% of Americans believe the government has “not effectively addressed veterans’ transition to civilian life.” And 60% of veterans say they’re not satisfied with the VA’s current approach and success rate for PTSD treatment for veterans.
Mission Roll Call is a nonpartisan movement providing veterans with a powerful, unified voice that is heard by our nation’s leaders and communities.
Sign up for our newsletter, follow us on social media, or consider donating to support our mission. You can also write a letter to your Senator or Congressperson and ask them to support a specific veterans’ issue. You can find out more about what’s going on at Capitol Hill by signing up for our newsletter.

Conclusion
Whether in public service, the private sector, or volunteerism, veterans continue to display their unwavering dedication to those around them. And the unique set of tools and skills cultivated during their time of service continues to pay dividends in service of the American people.
This Veterans Day, commit to doing one thing to show gratitude to a veteran you know – or haven’t met. But don’t stop there. We shouldn’t only thank veterans on one day of the year. A “thank you” is always appropriate – and appreciated.
Service animals can play a pivotal role in aiding veterans who face physical and mental challenges due to their military service. These animals, often dogs, are extensively trained to provide tailored support. Around 27% of veterans reported having a service-connected disability as of August 2022, and at least 7% of veterans will experience post-traumatic stress (PTS) at some point in their lives.
For veterans with physical disabilities, service animals can assist with tasks such as retrieving items, opening doors, and maintaining balance — restoring a sense of autonomy. They can also play an important role in supporting veterans’ mental health. For those dealing with conditions like PTS, anxiety, and depression, these animals can detect signs of distress and intervene appropriately. Although the Americans with Disabilities Act (ADA) provides that dogs and miniature horses can become service animals, this article will focus on service dogs and answer common questions, such as:
- What are service animals?
- How do service animals help veterans?
- Does the VA provide service animals to veterans with PTS?
- What is the Service Dog Assisting Veterans (SAVES) Act meant to do?
- How can we support veterans in need of service animals?
What are service animals?
If a veteran is experiencing significant physical, mental, or mobile limitations in their day-to-day life, they may qualify for a service dog. The U.S. Bureau of Labor Statistics reported that about 27% of veterans have a service-connected disability as of August 2022 — with rates particularly high among post-9/11 veterans. Moreover, according to the Department of Veterans Affairs (VA), at least 7% of veterans overall will experience post-traumatic stress (PTS) at some point in their lives compared to 6% of non-veterans. For post-9/11 veterans, the rate is 29%, and 15% have reported symptoms in the last 12 months.
A veteran service animal is a highly trained companion for military veterans dealing with service-related challenges. Typically dogs, these animals learn tasks like retrieving objects, opening doors, and providing balance support to enhance the veteran’s independence. Beyond physical assistance, they can recognize signs of distress, waking a veteran up from nightmares, calming panic attacks, and helping reduce feelings of isolation and depression.
There are different categories of service dogs, with some capable of fulfilling multiple roles. In contrast to emotional support dogs, service dogs undergo intensive training programs to equip them for aiding the veterans they are matched with. Some types of service dogs include:
- Psychiatric service dogs trained to assist those with PTS, severe anxiety, and major depression;
- mobility assistance dogs for those with physical limitations;
- guide dogs for the visually impaired;
- hearing dogs for the hearing impaired; and
- diabetes assistance dogs that are scent-trained to detect blood sugar levels.
Veterans enrolled in VA healthcare who meet certain requirements can be pointed to organizations that match them to the right animal based on their needs, medical history, and lifestyle. These animals are not mere pets; they serve as a crucial link to normalcy, independence, and psychiatric healing for those who served their country.
The deep bond between a veteran and their service animal can even be therapeutic, providing a sense of purpose and responsibility that traditional treatments do not. For example, for a veteran experiencing panic attacks, a service dog can be a grounding presence and companion, helping to alleviate anxiety. Moreover, they can help combat isolation and encourage veterans to be more engaged and active in their daily lives. Through their training and companionship, veteran service animals offer a path to an improved quality of life for veterans who have made significant sacrifices.
How Service Animals Help Veterans
The bond formed with a service animal can often transcend companionship and become a source of healing and emotional support. Research has shown connections between the presence of a service dog, specifically one for PTS, and better regulation of the stress hormones associated with anxiety and PTS. Therapy is usually the “first-line approach” for veterans with PTS, and the success largely depends on the severity of symptoms. For long-term conditions, treatment often also includes medication and other lifestyle changes. To this end, service dogs can be a great complementary — or replacement — treatment, potentially keeping the veteran from having to increase medication doses, and reducing suicidal ideation.

Only about 50% of veterans — around 9 million — are enrolled in VA healthcare or affiliated with a veteran service organization. Of the 6 million veterans served by the VA healthcare system in fiscal year 2021, about 10% of men and 19% of women were diagnosed with PTS. Data from the RAND Center for Military Health Policy Research shows that less than half of veterans in need of mental health services receive treatment. Of those who do receive treatment – for PTS and major depression specifically — less than one-third are getting evidence-based care.
Moreover, the veteran community consistently deals with a concerning rate of suicide. America’s Warrior Partnerships interim report suggests at least 40-44 former service members die by suicide or self-harm every day. And while suicide should not only be looked at through the lens of mental health issues, as there are a range of contributing factors, PTS and other mental health conditions do play a role. But even if those issues are not a determining factor in a veteran’s dark spiral with suicidal ideation, when someone gets to that point they usually feel alone and unloved. A service dog can provide a powerful backstop to those thoughts.
When it comes to conditions like depression, anxiety, and PTS, there’s a need for effective holistic, alternative treatments. Ongoing research on the human-animal bond shows service animals can help ease PTS symptoms, reduce anxiety, and even improve sleep for veterans who have experienced trauma. By helping to foster healthy routines, a sense of independence, and emotional connection, service animals can also contribute to veterans with service-connected disabilities’ reintegration into society. These animals serve as steadfast allies, facilitating veterans’ journeys toward improved well-being and an enhanced quality of life.
Does the VA provide service animals to veterans with PTS?
For service animal-related benefits, a veteran must first be enrolled in VA healthcare. In certain cases, VA benefits will cover care and equipment for service dogs. Veterans must first meet with their healthcare provider to discuss their physical or mental health limitations to determine if a service dog will be an appropriate treatment approach. Each case is individually reviewed by a clinician to assess the goals to be accomplished by getting a service dog and the ability and means of the veteran to care for the dog.
Upon approval for a service dog, veterans are referred to Assistance Dogs International accredited agencies or International Guide Dog Federation accredited agencies to be paired with the right type of service dog. From there, they can also have their service dog enrolled in Veterinary Health Benefits now, thanks to recent expansions in the VA benefits. This includes comprehensive treatment and wellness checks, emergency care, immunizations, and illness treatment for the dog that will be serving the veteran.
They are also provided with the proper equipment, such as a harness or vest, with the hope of ensuring that the service dogs remain in good health to best serve veterans.
VA healthcare currently does not cover training, medications, food, grooming, or other ongoing expenses. Promisingly, the Puppies Assisting Wounded Servicemembers for Veterans Therapy (PAWS) Act — signed into law on August 25, 2021— requires the VA to conduct a five-year pilot program to provide service dog training for eligible veterans experiencing PTS as part of a “complementary and integrative health program.” The program is meant to explore the benefits of service dog training, and based on the data, the training could potentially be included in comprehensive healthcare benefits for service animals in the near future.
The Importance of the SAVES Act
The Service Dogs Assisting Veterans (SAVES) Act is legislation meant to help match veterans with a service dog in an effort to better support the mental health of former service members.
Introduced in June 2021 and led by Senators Thom Tillis (R-N.C.) and Richard Blumenthal (D-Conn), the bill would establish a program to “award grants to nonprofit organizations that provide and place service animals with veterans while also building on the PAWS Act, which could open the door for the VA to assist in the training of service animals.
An estimated 20% of Iraq and Afghanistan war veterans in particular are experiencing PTS, and more than 450,000 service members have been diagnosed with a traumatic brain injury over the last 20 years— underscoring the need for a proactive approach to ensuring the health and well-being of our country’s former service members. In fact, Mission Roll Call’s 2022 annual research survey found that almost half of the American public (46% ) believes the federal government could do more to support veterans’ healthcare and mental health needs. Initiatives like the SAVES Act are a step in the right direction.
How can we support veterans in need of service animals?
As individuals, we can play a role in encouraging the well-being, mobility, and overall quality of life for veterans experiencing mental health challenges or physical service-related disabilities. Not only does checking in as a supportive loved one help, but informing and connecting veterans in your life to options for service animals could make a huge difference as well.
There are several organizations that train and provide service animals for veterans, such as K9s for Warriors, the nation’s largest provider of trained service dogs for veterans with PTS, traumatic brain injury, or military sexual trauma. Additional organizations include SemperK9, America’s Vet Dogs, Patriot Service Dogs, and Canine Companions.
Mission Roll Call continues to partner with veteran service organizations to raise awareness and meet the needs of our nation’s former service members. Specifically, we advocate for proactive initiatives and policies that can help prevent suicide among veterans; ensure veteran access to quality healthcare, and address the inequities underserved veteran communities are experiencing.
Learn more about our mission and get involved by signing up for our newsletter, participating in our member polls, or making a donation. You can also contact your congressional representative and urge them to support and prioritize legislation such as the SAVES Act and other policies that can make a positive impact on the lives of our nation’s veterans.
The PACT Act was signed into law by President Joe Biden in August 2022, instituting the largest expansion of healthcare benefits for veterans in a generation. An estimated 3.5 million veterans have been exposed to burn pits — open-air pits often used to burn chemical waste — and other harmful substances since the 9/11 attacks. Symptoms can include chronic headaches, fatigue, throat burning, difficulty breathing, skin rashes, and in severe cases, can lead to various cancers and other illnesses.

The legislation was an important step in right-sizing healthcare benefits for former service members impacted by toxic exposure, especially as more research points to connections between chemicals in military environments and a variety of illnesses.
Now, one year since the law was passed, we take a look at the progress, highlight ongoing needs in veterans’ healthcare, and answer the following common questions:
- What is the PACT Act?
- How can veterans get PACT Act benefits?
- What disabilities are covered under the PACT Act?
- How can we support veterans who have been exposed to toxins?
The brave women and men who honorably served deserve access to sufficient benefits, proper treatment, and providers specializing in caring for the wounds they bear as a result. The PACT Act was a major step in the right direction; now it’s up to lawmakers and the VA to see that it’s implemented properly and all veterans exposed to toxic substances are made aware of the benefits available to them.
What is the PACT Act?
The PACT Act — short for “Promise to Address Comprehensive Toxics” – was signed into law on August 10, 2022, by President Joe Biden. It expands VA healthcare and benefits for veterans exposed to Agent Orange, burn pits, and other toxic substances. The bill is considered the largest healthcare and benefits expansion in VA history. Since its passage, more than 3 million veterans have received VA’s new toxic exposure screenings with about 42% (1.3 million) reporting a “concern of exposure.” Specifically, the law does the following:
- expands and extends eligibility for VA healthcare-enrolled veterans of the Vietnam, Gulf War, and post-9/11 eras who have experienced toxic exposure;
- requires the VA to provide a toxic exposure screening to all veterans enrolled in VA healthcare;
- increases the number of presumptive conditions for burn pits, Agent Orange, and other toxic exposures with more than 20 additional conditions;
- includes more “presumptive-exposure” locations for radiation and Agent Orange; and
- aims to improve research, education, and treatment related to toxic exposures.
The objectives of the PACT Act are crucial to the well-being of so many of our former service members. Biden, whose eldest passed away from cancer years after deploying to Iraq, stated to veterans upon signing the bill: “We owe you. You’re the backbone. You’re the steel. You’re the sinew. You’re the very fiber that makes this country what it is.”
Indeed, so many that have worked to secure our nation at home and abroad were inadvertently exposed to toxins that could negatively impact their health. And unlike the threats of combat, chemical exposure can easily be overlooked. For example, many veterans of the Global War on Terror who served in Iraq and Afghanistan were exposed to toxic fumes from burn pits. These open-air pits would be used to discard chemical waste, human waste, medical equipment, tires, and plastics on military bases. Some only discovered later that there were airborne substances that could be harmful to their health.
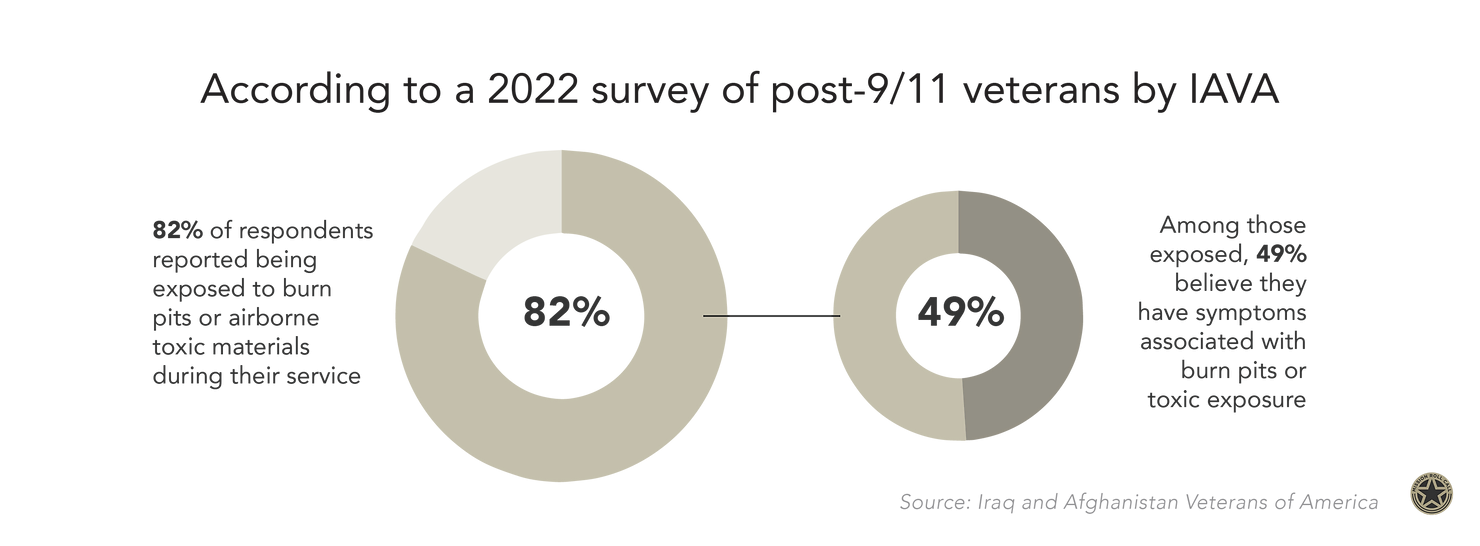
According to a 2022 survey of post-9/11 veterans by Iraq and Afghanistan Veterans of America (IAVA), 82% of respondents reported being exposed to burn pits or airborne toxic materials during their service, and among those exposed, 49% believe that they have symptoms associated with burn pits or toxic exposure.
Moreover, a 2022 Mission Roll Call poll found only 12% of veterans with exposure to toxic substances had completed the VA’s Airborne Hazards and Open Burn Pit Registry, suggesting there may be gaps in the agency’s estimates and related research. Promisingly, though, 72% of respondents reported an intention to submit a disability claim for toxic exposure, which can help them get appropriate care.
Veterans with toxic exposure can experience a number of immediate and long-term health problems, including chronic fatigue, headaches, sudden skin rashes, and cancer. Certain conditions can go undetected without proper screening, and those who are unaware of the chemicals present in their environment may be less likely to connect health symptoms to their service experiences. Therefore it’s imperative that the VA and lawmakers build awareness around the expansions to VA health benefits via the PACT Act and the importance of veterans taking part in the free screenings.
How can veterans get PACT Act benefits?
Veterans enrolled in VA healthcare can file a disability claim to apply for PACT Act benefits, including treatment coverage and compensation in some cases. There is no deadline to apply for related benefits, but veterans who apply or submit an “Intent to File” by August 9, 2023, can have their benefits backdated to August 10, 2022 — the day President Biden signed the PACT Act into law. The VA is even hosting a nationwide “Summer VetFest” to encourage veterans to apply. The outreach initiative will include over 50 events across the country to “inform veterans, their families, caregivers, and survivors about the PACT Act.”
In the past, proving that toxin exposure caused an illness was difficult, and veterans often found it extremely challenging to get proper healthcare benefits for illnesses caused by those toxins. For instance, prior to the passage of the PACT Act, around 70% of disability claims related to burn pit exposure were denied by the VA. Thankfully, more scientific research and awareness are increasing understanding of the connections between toxin exposure and illness, particularly from burn pit fumes, radiation exposure, and Agent Orange exposure.
Chemical and toxic substance exposure varies by service era, and the list of contaminants includes smoke from burn pits used throughout Afghanistan and Iraq, Agent Orange residue near work sites in Vietnam, and elevated radiation levels and contaminated water at military bases. Some common symptoms of toxic substance exposure are chronic fatigue, headaches, skin rashes, throat irritation, or trouble breathing.
Disabilities Covered Under the PACT Act
Over 20 “presumptive conditions” connected to exposure to burn pits and other toxic substances have been added through the PACT Act, expanding VA benefits for Gulf War era and post-9/11 veterans. Presumptive conditions are diagnosed disabilities that are presumably caused by a veteran’s military service.
- Presumptive cancers include: Gastrointestinal cancers, lymphoma, head cancers, neck cancers, reproductive cancers, respiratory cancers, brain cancers, kidney cancers, pancreatic cancers, melanoma, and glioblastoma.
- Presumptive illnesses include: Chronic obstructive pulmonary disease (COPD), asthma diagnosed after service, chronic bronchitis, chronic rhinitis, chronic sinusitis, constrictive bronchiolitis or obliterative bronchiolitis, emphysema, granulomatous disease, interstitial lung disease (ILD), pulmonary fibrosis, pleuritis, and sarcoidosis.
- Presumptive conditions from Agent Orange include: High blood pressure (hypertension), diabetes mellitus type 2, ischemic heart disease, monoclonal gammopathy of undetermined significance (MGUS), hypothyroidism, parkinsonism, and Parkinson’s disease.
Additionally, Vietnam-era veterans along with nuclear/radiation-exposed veterans and military families exposed to contaminated water at Camp Lejeune are also eligible. And though eligibility depends on service history and other factors, veterans are encouraged to apply no matter their separation date.
Through the PACT Act, many veterans can get free VA healthcare for any condition related to service for up to 10 years from the date of their most recent discharge or separation. Veterans can also enroll at any time during this period and get care, but may owe a copay for some care. Those enrolled will receive an initial screening and a follow-up screening at least once every five years.
As of May 2023, the VA had processed 252,000 of the 546,000 PACT Act claims filed by veterans, approving nearly 80% for one or more conditions. And of 14,000 survivors of veterans who have filed claims for disability compensation, 6,000 cases have been reviewed, resulting in benefits to 3,600 survivors — reflecting increased efficiency and notable effort from the agency.
How can we support veterans who have been exposed to toxins?
Even though PACT Act benefits have rolled out over the last year, there is still time to inform veterans of what they may be eligible for. As individuals, we can play a role in helping ensure former service members with toxic exposure get the care and support they need. If you know veterans of any of the aforementioned service eras, point them to the latest news via the VA on PACT Act benefits and encourage them to get a free toxic exposure screening at a local VA facility.
As of 2021, there were a reported 16.5 million former service members across the country, and nearly half are unaffiliated with VA. Part of the issue is that veterans can easily become overwhelmed navigating the complex system of VA benefits. The Veterans Health Administration (VHA) — a branch of the VA led by the Under Secretary for Health of Veterans Affairs — oversees and carries out the healthcare program of the VA. As the largest integrated healthcare system in the U.S., it provides care to over 9 million veterans at 1,298 healthcare facilities across the country.
Even with the expansion of benefits based on the PACT Act, we should urge the VA to develop initiatives to better explain VA benefits prior to service members’ military separation. We must also call on Congress to prioritize ongoing oversight of the VA’s implementation of the PACT Act along with policies like the MISSION Act, which is aimed at strengthening comprehensive healthcare for veterans. Ensuring the VA adheres to the standards and objectives outlined in each law is key to successful outcomes in the long term.
Mission Roll Call continues to advocate for each of these measures with the goal of ensuring all veterans have access to quality care. The passage of the PACT Act was a great development, and it has already impacted millions of veterans with toxic exposure. The wounds of service members are not always apparent, and it’s vital to make as many veterans as possible aware of the ways chemical toxins could be affecting their health. To keep up the momentum, share this blog post with veterans in your community and use your voice on social media to help spread awareness.
Post-traumatic stress (PTS) is a condition that can develop after witnessing or experiencing a tragic or traumatizing event. The Department of Veterans Affairs (VA) estimates that seven out of every 100 veterans will experience PTS at some point in their lives, compared to six out of 100 non-veteran adults. The condition is also more common among female former service members: 13% are expected to have PTS in their lifespan compared to 6% of male veterans.
As we observe PTS Awareness Month, it’s a great time to explore how it impacts our nation’s veterans and ways we can better support them. Moreover, it’s an opportunity to highlight current gaps in mental health support and care for former service members that can create hurdles in treatment.
In this article, we’ll explore the following questions:
- What is post-traumatic stress (PTS)?
- Are veterans at higher risk for PTS?
- How many veterans are experiencing PTS in 2023?
- What PTS treatments are available for veterans?
- How can we support veterans experiencing PTS?
Overall, veterans are experiencing PTS at higher rates than the general public, and there’s more that can be done by the VA and lawmakers to provide former service members with adequate, comprehensive assistance. At the same time, we must negate harmful notions around veterans’ mental health. As individuals, we can help by dispelling inaccurate stereotypes and pointing veterans with PTS — something anyone, including civilians, can experience after trauma — to helpful resources for mental health care.
What is post-traumatic stress (PTS)?
Post-traumatic stress (PTS) is a mental health condition that can develop after going through or seeing traumatic events such as a natural disaster, car accident, explosion, abuse, etc. It’s a common and often adaptive response to an abnormally stressful situation. Veterans are considered to have a higher risk of developing PTS than the general public due to unique stressors associated with combat and military life. Symptoms of post-traumatic stress may include:
- Flashbacks — memories of the traumatic event that come back suddenly and unexpectedly
- Nightmares — dreams about the traumatic event that occur over and over again
- Avoidance — avoiding places, activities, or people associated with the trauma
- Physical reactions — exhibiting physical signs of stress, such as a racing heart, sweating, anxiety, and nervousness.

Although symptoms of PTS can subside within weeks after the event, it’s recommended that anyone exhibiting these reactions speak with a healthcare provider to be evaluated for appropriate treatment and support.
Post-Traumatic Stress (PTS) vs. Post-Traumatic Stress Disorder (PTSD)
PTSD has become somewhat of a catchall term for all types of post-traumatic stress symptoms, but there are important differences between PTS and PTSD that should be understood.
PTS is a normal, and at times adaptive, response to trauma. It’s not a mental illness but something that many people — not just service members and veterans — experience after facing an extremely stressful event in their lives. Common occurrences like a sports accident or clumsy fall can trigger PTS, as well as more unusual events like war tragedies or an assault. Unlike PTSD, PTS is not chronic, and people can usually find relief in the short term.
PTSD is a medically-diagnosed condition and should be treated by a clinician. Symptoms can be chronic — lasting a year or more and requiring ongoing medical attention. PTSD symptoms typically develop within one month, and, though similar to symptoms of PTS (flashbacks, nightmares, racing heart, etc.), they can be more intense and long-lasting. According to the VA, about 10% of male veterans and 19% of female veterans who used VA healthcare in fiscal year 2021 were diagnosed with PTSD.
The term PTS is also used instead of PTSD by some (including Mission Roll Call) to alleviate the stigmas around having a “disorder” and to dispel myths of “broken veterans.” For example, a 2021 study by the University of Cincinnati looked at common stigmas veterans face and found that “depictions of veterans in news media and pop culture often carry negative associations such as poor mental health or violence.”
Facing these preconceived notions can make veterans reluctant to share their mental health challenges with friends and family or seek help. As such, the term PTS will be used in most cases throughout the rest of the article.
Are veterans at higher risk for PTS?
While PTS is a psychological injury that can affect anyone who experiences trauma, veterans are more likely to develop PTS than non-veterans. The VA estimates that at least seven out of every 100 veterans will experience PTS at some point in their lives. And RAND Center for Military Health Policy Research data has found that up to 20% of service members returning from the Global War on Terror (GWOT) have experienced PTS.
Combat experience in particular can make a person more sensitive to loud noises or bright lights, trigger insomnia and trouble sleeping, and make everyday situations feel more stressful than they did beforehand.
What’s more, veterans may face distinct barriers to accessing adequate mental health treatment. Research shows that less than half of veterans in need of mental health services receive treatment, and of those who do — for PTS and major depression — less than one-third receive evidence-based care.
There are also links between PTS and high suicide rates among veterans.
While suicide should not only be looked at through the lens of mental health — since a variety of other factors can play a role, the VA’s data shows the veteran suicide rate is 52.3% higher than non-veterans. America’s Warrior Partnerhip’s research even suggests the rate may be higher than the VA’s estimate, with their 2022 interim report pointing to at least 40-44 former service members dying every day by suicide or self-harm.
These concerning statistics highlight the need for comprehensive mental health care that takes a holistic approach to veterans’ needs. More than that, service members must be given proper resources and information on health benefits prior to military separation. Specifically, they should be provided with clear roadmaps for identifying symptoms and finding treatment for PTS and other mental health challenges.
PTS Rates Among Veterans in 2023
According to the VA, 7% of veterans will experience PTS at some point in their lives.
Veteran PTS rates are often categorized by service era, and prevalence among post-9/11 veterans tends to be higher, with 15% experiencing PTS in the last 12 months and 29% expected to experience it at some point in their lives.
A Pew Research study found that 36% of post-9/11 veterans believe they have suffered from PTS. And, being more likely to have been deployed and to have seen combat than veterans of other eras, nearly half said they had “emotionally traumatic or distressing experiences related to their military service.”PTS is also more common among female veterans, as 13 out of every 100 are expected to have PTS in their lifespan compared to six out of every 100 male veterans.
The following data is provided by the VA and was compiled from a large study of veteran demographics across the U.S.
| Service Era | PTS in the last 12 months | PTS at some point in life |
|---|---|---|
| Operations Enduring Freedom (OEF) and Iraqi Freedom (OIF) | 15% | 29% |
| Persian Gulf War | 14% | 29% |
| Vietnam War | 5% | 10% |
| World War II and Korean War | 2% | 3% |
Interestingly, former service members who use the VA healthcare system are more likely to be diagnosed with PTS than those who use community health services. This could be partly due to the fact that the VA screens all patients for PTS symptoms. Veterans who have been deployed and experienced combat during their service are also more likely to develop PTS than those who have not. Other scenarios that can exacerbate risks are: discharging a weapon, witnessing a death, being attacked, lack of support in transitioning from the military, and losing a sense of camaraderie and purpose post-deployment.
PTS Rates Among Veterans of the Global War on Terror
PTS has come to be known as the “signature wound” of veterans who served in the Global War on Terror (GWOT).

The VA reports that 29% of veterans who served in Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF) – in Iraq and Afghanistan – will exhibit PTS symptoms at some point. And the Wounded Warrior Project’s 2022 survey of post-9/11 veterans found that 75.9% reported experiencing PTS; 49.8% reported moderate to severe symptoms of two or more mental health conditions, such as depression and anxiety; and 28.3% reported having suicidal thoughts in the last 12 months. The survey consistently shows that these veterans experience PTS at a much higher rate than the VA estimates as well.
The GWOT also saw a rise in improvised explosive devices (IED) and traumatic brain injury (TBI) impacting service members. Coupled with the war’s protracted length, all of these circumstances can play a role in elevating the risk of PTS and other mental health challenges for veterans.
What PTS treatments are available for veterans?
Therapy is usually regarded as a “first-line approach” for veterans with PTS. The success of PTS treatment depends on the severity of symptoms and how long they have been present. For long-term conditions, typically associated with PTSD, treatment often also includes medication and lifestyle changes. Only 50% of veterans — around 9 million — are enrolled in VA healthcare or affiliated with a veteran service organization. And of the 6 million veterans served by the VA healthcare system in fiscal year 2021, about 10% of men and 19% of women were diagnosed with PTSD.
Without the support they need, in the VA or their community, many veterans may turn to self-destructive coping mechanisms. A holistic approach is needed to combat the feelings of isolation, depression, and potential suicide ideation that can come with PTS. It is important for veterans to have a strong network during this process; having people to check in with, spend quality time with, or who serve as mentors can be a vital source of encouragement.
In the case of PTSD diagnosis, the VA offers three forms of therapy: cognitive processing therapy (CPT), prolonged exposure therapy, and eye movement desensitization and reprocessing (EMDR). Over 50% of patients who receive one of these three therapies will find relief, according to the National Center for PTSD. Or with medication alone, 42% have been found to achieve remission — though there have been concerns in the veteran community about negative side effects associated with some prescribed medications.
Ensuring positive outcomes must also include improving VA mental health services with practitioners that specialize in veterans’ care; implementing increased community care provisions as outlined in the MISSION Act, so that veterans can find quality care within a reasonable timeframe or distance; rightsizing disparities in VA healthcare facilities in underserved areas; and improving transition assistance programs to ensure veterans are fully aware of the healthcare benefits available to them upon exiting the military.
How can we support veterans experiencing PTS?
Mission Roll Call 2022 annual research survey on Americans’ attitudes on a range of veterans’ issues found 60% believe veterans deal with post-traumatic stress (PTS) a lot more than their civilian counterparts. And nearly half (46%) of U.S. adults believe the federal government has “not been very effective” in dealing with veteran healthcare, including mental health support. Considering this, there is ample room for individuals to play a role in supporting our nation’s veterans, especially those experiencing PTS.

We can point veterans in our lives to helpful resources and information on healthcare benefits they may be eligible for. The VA provides general and specialty mental health services, including treatment for PTS and other conditions. Moreover, if you have a veteran in your life showing symptoms of PTS, you can:
- Learn as much as you can about PTS. Knowing how it affects people may help you better understand how to support your loved one or friend.
- Encourage them to speak to healthcare providers who specialize in veterans’ needs and help them find a therapist if recommended by a doctor.
- Participate in physical activities with them. Consistent exercise is important for overall health, and activities like jogging, taking walks, or going for a bike ride can help improve mental health.
- Provide a listening ear and let the veteran know that you are there for them if they need to talk about their experience.
- Help them connect with other veterans in the same situation (via online forums, Facebook groups, etc.).
Good relationships can have a positive impact on veterans’ mental and physical health. Organizing support groups, spending quality time with a veteran experiencing PTS, or volunteering for a veteran-serving organization are all great ways to show support. The VA’s National Center for PTSD also has information for veterans, service members, families, and providers, and the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury offers fact sheets and resources on PTS care as well.
Finally, you can encourage veterans you know to share their stories with Mission Roll Call, as we make ongoing efforts to present and advocate for the needs of veterans across America.
Conclusion
PTS is a condition that can affect veterans’ quality of life at higher rates than the general population. This month, as we raise awareness around PTS, let’s make it a point to learn more about how it impacts our veterans. There are many treatment options available that can help relieve symptoms and feelings of isolation. It’s important to remember that PTS is not a sign of weakness or brokenness but an adaptive psychological response to trauma. Therefore, we must ensure our brave veterans — who have selflessly served our nation — are not met with stigmas and barriers but instead have access to the best care, support, and resources.
Healthcare access has long been an issue for our nation’s veterans, and the MISSION Act — signed into law on June 6, 2018 — was a step toward reducing barriers to quality care for former service members. Aimed at strengthening the Department of Veterans Affairs (VA) healthcare system, the law expanded community care provisions to help ensure veterans can find appropriate medical care within a reasonable distance and/or timeframe.
Despite the significant contributions veterans make to society during and after service, they can face challenges navigating bureaucracy around VA healthcare & benefits. Additionally, they may experience disparities in local VA facilities, long wait times for appointments, or a lack of providers specializing in veterans’ needs.
As we look at the progress made since the MISSION Act was passed, we’ll also break down the current roadblocks to the law’s effectiveness and answer the following questions:
- What is the MISSION Act?
- Who is eligible to benefit from the MISSION Act?
- What progress has been made since the MISSION Act was signed?
- What else should Congress and the VA do to improve healthcare for veterans?
What is the MISSION Act?
The MISSION Act was signed into law on June 6, 2018, to establish a new community care program for the VA healthcare system, among other provisions. Its aim is to strengthen nationwide VA healthcare overall, and a few key objectives are to:

- improve the VA’s ability to recruit and retain clinicians;
- increase veteran access to community care providers;
- provide “Anywhere to Anywhere” telehealth support across state lines;
- reduce wait times for appointments at VA healthcare facilities;
- ensure veterans can get care within a reasonable driving distance; and
- expand urgent care benefits within the VA’s network of urgent care providers.
The Veterans Health Administration (VHA) is a branch of the VA that oversees and carries out its healthcare program. The VHA system provides care to over 9 million veterans enrolled in VA healthcare at 1,298 healthcare facilities, including 171 VA medical centers and 1,113 outpatient sites.
A major step in reaching the goals of the MISSION Act was centered on revising the department’s private-sector healthcare programs for veterans by consolidating a number of non-VA affiliated healthcare options into a single community care program. This was intended to provide more healthcare options to veterans while still having the costs covered by the department.

Today, the renewed and expanded VA community care program is making strides, but there’s much work to be done in ensuring veterans have access to quality healthcare within a reasonable timeframe or distance. The availability of comprehensive mental health support is among the crucial needs that have yet to be sufficiently met.
For instance, veterans faced nearly 20 million canceled or delayed appointments during the COVID-19 pandemic. On top of that, the fallout from the U.S. withdrawal from Afghanistan in August 2022 reportedly contributed to a spike in crisis hotline calls, as former service members “struggled to process the unfolding events.”
This underscores the need for comprehensive medical care that includes proper mental health care.
In fact, a study from the RAND Center for Military Health Policy Research shows that less than half of veterans in need of mental health services receive treatment. And of those who do, less than one-third get evidence-based care. The Center’s research also found that deployment “increases risks of mental health conditions and related problems among veterans who have served since the September 11, 2001, attacks.”
In light of this, the VA must work to improve veteran access to medical care and mental wellness support by increasing the number of trained mental health providers; creating initiatives to educate and inform veterans about treatment options; standardizing performance measurements for VA community care facilities; and providing evidence-based treatment and therapies for veterans with mental health conditions. Additionally, Congress must put in place measures to see to it that the MISSION Act’s aims are being fulfilled by the VA, with clear-cut plans to resolve the current gaps in veteran care.
Who is eligible to benefit from the MISSION Act?
Veterans enrolled in the Department of Veterans Affairs (VA) may be eligible for at least basic VA healthcare coverage and therefore benefit from the care improvements outlined in the MISSION Act. The Basic Medical Benefits Package includes preventive, primary, and specialty care, as well as diagnostic, inpatient, and outpatient care services.
And under the newly-established Veterans Community Care Program — an outcome of the MISSION Act — veterans can work with their VA healthcare provider to see if they are eligible to receive care outside the VA’s system. In most cases, eligibility is based on one or more of the following criteria:
- Needing a service not available at any VA medical facility.
- Living in a U.S. state or territory without a full-service VA medical facility. (e.g., U.S. territories, Alaska, Hawaii, etc.)
- Qualifying under the “grandfather” provision related to distance eligibility according to the Veterans Choice Program.
- Verification that the VA cannot offer care within certain designated access standards.
- Having the veteran and referring doctor agree it is in the best medical interest of the veteran to receive community care.
- Having the VA determine that an affiliated provider is not offering care that complies with the VA’s quality standards.
Though these provisions and clarifying updates are a step in the right direction, there are many veterans who may be left out of the improvements to VA healthcare benefits.
According to the U.S. Census Bureau, there were a reported 16.5 million veterans across the country as of 2021. And with just over 9 million veterans enrolled in the VA healthcare program, nearly half of all veterans are unaffiliated and therefore not able to benefit from the MISSION Act’s agenda.
Part of the issue is a lack of understanding of VA coverage and unclear roadmaps for enrollment as service members transition from military to civilian life. Veterans can easily become overwhelmed navigating the complexities of VA healthcare.
According to feedback in the Journal of Veteran Studies, many former service members expressed a desire to see the VA change its broad approach to transition assistance. In their opinion, this would include putting more emphasis on ways to secure practical needs like healthcare and mental health services.
Moreover, the Military Family Advisory Network (MFAN) 2021 survey of more than 8,000 veteran and military families found that access to the VA healthcare system was one of the respondents’ top concerns. Specifically, the MFAN report reveals negative experiences with providers, poor quality of care, trouble scheduling appointments, and a lack of available appointments were issues frequently cited among the feedback on VA healthcare and mental healthcare services.
As we reach another anniversary of the MISSION Act’s passage, it’s an opportunity to assess how well the law’s guidelines are being implemented. We must ensure that veterans are not only aware of the healthcare benefits that are available to them but that they are experiencing tangible improvements while navigating the VA healthcare system.
What progress has been made since the MISSION Act was signed?
The passage of the MISSION Act in 2018 was an important step toward providing comprehensive, quality healthcare for veterans. Since then, the expansion of community care options and revised urgent care benefits were among the most significant changes. This has helped establish clear eligibility criteria for veterans to receive care outside of the VA system and allowed for quicker access to treatment through the updates to urgent care services.
Although progress has been made, there is still much to be done to ensure former service members can access the care they need.
Current roadblocks to the MISSION Act’s effectiveness reflect a lack of congressional oversight and assurance of the VA’s adherence. For instance, USAToday reports that “VA administrators are overruling doctors’ judgments and preventing them from sending their patients outside the VA health care system.” The allegations are based on a review of thousands of medical records and department documents, along with interviews with dozens of patients, providers, and veterans healthcare advocates.
Lengthy appointment wait times are especially an issue for veterans living outside of urban areas.
Despite 4.7 million veterans — close to a quarter of all veterans — living in rural communities, there are significant healthcare disparities in these areas.
A February 2023 report by the Government Accountability Office (GAO) explains how VHA officials confirmed “veterans living in rural areas face unique barriers to accessing mental health care” and that it’s often due to “staff shortages in rural facilities and transportation issues.” Based on the VHA’s 2021 data, GAO found that rural veterans used outpatient care at a much lower rate than urban veterans, with only 21% of rural veterans obtaining services at these facilities compared to 79% of urban veterans.
With proper congressional supervision and clear roadmaps to achieve the goals of the MISSION Act, we can see much-needed progress on veterans healthcare barriers going forward. There have already been a few promising legislative steps to improve veterans healthcare over the past year, including:
Support for Veterans in Crisis: The Biden administration announced in January 2023 that veterans in suicidal crisis can receive free emergency medical care at any VA or private care facility.
The HEALTH Act: Introduced in April 2023, this bill aims to “protect and expand access to care for veterans, safeguard veterans’ ability to choose their own providers and require VA to improve the quality of care veterans receive.”

The Protecting Veteran Community Care Act: Montana Rep. Ryan Zinke introduced this legislation in May 2023, with the goal of streamlining current veteran community care options and allowing for expedited residential healthcare options where appropriate.
VA Mobile Application Launch: The VA launched a mobile application in August 2022 named “VA: Health and Benefits,” intended to centralize veterans’ health and benefits information and streamline navigation of VA services.
The PACT Act: The VA expanded benefits eligibility to over 3.5 million veterans after the PACT Act was passed in August 2022. It provides compensation and medical care to veterans who were exposed to toxic substances during their service.
What else should Congress and the VA do to improve healthcare for veterans?
Congress and the VA play an essential role in ensuring veterans have access to quality healthcare. Congress must see to it that the VA is implementing the MISSION Act standards properly. The VA must focus on right-sizing VA inequities in underserved areas, reducing wait times for connection to VA providers, improving mental health support, and increasing community care provisions — as outlined in the law.
And since navigating the healthcare system can be difficult or overwhelming for retiring or transitioning veterans, clear roadmaps are needed for service members transitioning to civilian life. Hence, the VA can also help meet the goal of strengthening its healthcare system by better explaining veteran benefits prior to service members’ military separation.
Making sure veterans can receive evidence-based mental health in a timely manner must be prioritized as well.
A February 2023 Mission Roll Call veterans poll asked if former service members with mental health challenges should be able to access the provider of their choice regardless of whether they are affiliated with the VA system. Out of 7,200 responses, 94% said yes — emphasizing the pressing need for strategic, timely community care expansion.

Finally, lawmakers and the VA should plan effective initiatives to increase VA enrollment among eligible veterans, as nearly half of the estimated 16.5 million veterans in our nation are unaffiliated with the VA. Overall, Congress must ensure the VA adheres to the MISSION Act’s access standards by establishing ongoing oversight of the progress made toward strengthening veteran healthcare.
Conclusion
The MISSION Act has presented opportunities for Congress and the VA to foster better healthcare standards for our veterans — and it’s what they deserve. The brave men and women who have served our country shouldn’t be met with hurdles to basic medical needs, nor should they be faced with disparities in their local communities. As we reflect on the progress made since the MISSION Act became law, let’s also remember and advocate for what still needs to be done to ensure no veteran is without access to proper healthcare and support.
