What Are the Barriers to Healthcare for Veterans?

Veterans have played a fundamental role in securing and bettering our nation. Yet many leave the military and find it difficult to access the healthcare benefits afforded to them. What’s more, limited Department of Veterans Affairs (VA) facilities, long wait times for appointments, or a lack of providers specializing in veterans care can exacerbate this issue.
Mission Roll Call’s August 2022 research survey found that 86% of U.S. adults believe Congress should provide quality and expedient healthcare for veterans. It’s crucial that we look at ways to ensure former service members are getting the health support they need.
In this article, we will explore the following topics:
- What healthcare benefits are available to veterans?
- What challenges do veterans face in accessing healthcare?
- What veterans healthcare issues should Congress and the VA prioritize?
- How can we assist veterans in getting the healthcare they need?
In recognizing the fact that veterans are facing difficulties in navigating VA healthcare benefits, lawmakers should prioritize effective implementation of the Mission Act, which is aimed at strengthening comprehensive healthcare for veterans; reducing wait times at VA facilities; and expanding mental health initiatives.
What healthcare benefits are available to veterans?
Veterans enrolled in the Department of Veterans Affairs (VA) may be eligible for at least the Basic Medical Benefits Package, which includes preventive, primary, and specialty care, as well as diagnostic, inpatient, and outpatient care services.
Veterans may also be entitled to other specialized healthcare programs.
For example, the VA provides general and specialty mental health services, including treatment for post-traumatic stress (PTS), substance abuse disorders, and military sexual trauma. These services are provided in the outpatient and inpatient mental health setting.
Outpatient dental care is also available to eligible veterans and may include preventive, diagnostic, surgical, and restorative treatments and procedures.
The Veterans Health Administration (VHA) is a branch of the VA led by the Under Secretary of Veterans Affairs for Health. The VHA oversees and carries out the healthcare program of the VA, and it is the largest integrated healthcare system in the U.S. The system provides care to over 9 million veterans enrolled in the VA healthcare program at 1,298 healthcare facilities, including 171 VA medical centers and 1,113 outpatient sites.
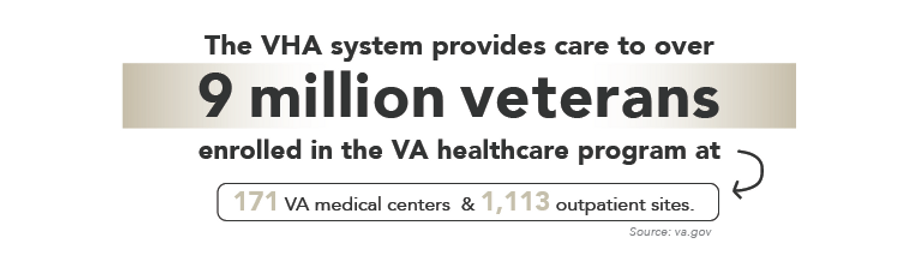
Even with an array of services available, navigating the healthcare system can be difficult or overwhelming for retiring or transitioning veterans. And although more than 9 million veterans are enrolled to receive services from the VHA, this only represents about half of the veteran population.
When it comes to mental health support, these statistics raise concerns.
Veterans are at a higher risk for PTS than nonveterans. The condition can develop after exposure to traumatic incidents and often leads to serious emotional anguish, mental stress, and an overall decreased quality of life for veterans.
Data from the RAND Center for Military Health Policy Research shows that less than half of veterans in need of mental health services receive treatment. And of those who do, less than one-third get proper, evidence-based care.
The VA must work to improve veteran access to care and benefits by providing comprehensive guidance on accessing healthcare services. Lawmakers need to look at the current gaps in veteran care and provide a clear-cut plan to resolve such disparities. This should include initiatives to improve mental health support, right-size VA equities in underserved areas, reduce wait times for connection to VA providers, and increase community care provisions.
What challenges do veterans face in accessing healthcare?

Many veterans face difficulties navigating VA healthcare, a lack of awareness of benefits or challenges in working through the complex system to receive them, inadequate mental health support, long wait times at VA facilities, and poor access to VA facilities in rural areas.
As of 2021, there were a reported 16.5 million former service members across the country, according to the U.S. Census Bureau.
With just upwards of 9 million veterans enrolled in the VA healthcare program, that means nearly half of all veterans are unaffiliated with VA. Part of the issue is the challenges in transitioning from the military to civilian life. Veterans can easily become overwhelmed navigating the complex system of VA benefits alongside practical difficulties like securing a job and housing.
The VA’s Transition Assistance Program, commonly known as TAP, takes a broad approach to assisting service members in their transition to life after service. But many veterans have said that more support should be given to help them adjust to new work environments, obtain affordable housing, and secure healthcare and mental health services.
The Military Family Advisory Network 2021 report on family support programming reflects this sentiment. Notably, in the survey of 8,638 military and veteran families, respondents listed access to the VA healthcare system as one of their top concerns. They cited trouble scheduling appointments and accessing care, negative experiences with providers, and poor quality of care. The lack of available appointments, in particular, was a recurring theme among the feedback on general VA healthcare and mental health care.
This is especially troubling when considering veterans are much more likely to die by suicide than nonveterans. America’s Warrior Partnership’s (AWP) 2022 interim report points to at least 40 to 44 former service veterans dying by suicide or self-injury each day.
It’s important to note that PTS and other mental health conditions are only part of the story, as studies have found connections to other factors like the impact of military culture, moral wounds, and sexual traumas. Still, without the proper support, many veterans in crisis can turn to harmful coping mechanisms, including self-harm. Hence, there is a pressing need for effective mental health support for veterans in crisis.
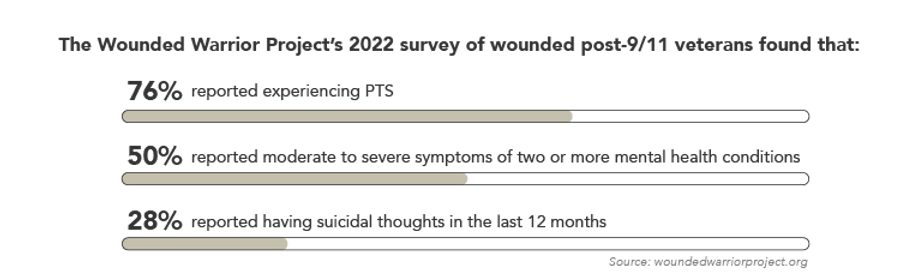
In fact, the Wounded Warrior Project’s 2022 survey of wounded post-9/11 veterans found that:
- 76% reported experiencing PTS;
- 50% reported moderate to severe symptoms of two or more mental health conditions, such as depression and anxiety; and
- 28% reported having suicidal thoughts in the last 12 months.
These results underscore the need for VA healthcare benefits to be improved and expanded to meet urgent needs. A February 2023 Mission Roll Call veterans poll asked if former service members with mental health challenges should be able to access the provider of their choice regardless of whether they are affiliated with the VA system, and out of 7,200 responses, 94% said yes.
What’s more, RAND Center for Military Health Policy Research findings suggest that less than half of veterans in need of mental health services receive proper treatment or evidence-based care.
Additional issues impacting veterans’ access to healthcare include long wait times and disparities in rural areas.
A 2014 audit pointed to 1,700 patients being put on secret waitlists for appointments at the Phoenix VA, and some even reportedly died waiting. While steps were taken since then to improve wait times, an April 2022 audit from the VA department’s inspector general found data is still being reported inconsistently and in a way that conceals true wait times.
This partially stems from the way the VA calculates how long veterans wait for care. A previous website used the “request date” of a practitioner or patient as the starting point. Now, the Access to Care site – launched in 2017 – goes by the “create date” for new patients, which is the date that a scheduler books an appointment.
The inspector general’s audit highlights a good example of the discrepancies this can lead to. For example, in the case of a veteran who saw a doctor on June 28, 2021, and was referred to see a cardiologist, this was logged on the same day as the “request date.” But a VA scheduler did not actually book an appointment until nearly a month later, and it was set for early September. The wait time, however, was logged as only 43 days instead of the actual total of 66 days.
Coupled with lengthy wait times are healthcare disparities in rural areas. Almost a quarter of all service members in the U.S. return from active duty to reside in rural communities, and there are currently an estimated 4.7 million rural veterans.
A Government Accountability Office (GAO) report released in February 2023 says VHA officials confirmed that “veterans living in rural areas face unique barriers to accessing mental health care” in particular due to “staff shortages in rural facilities and transportation issues.”
Also, in analyzing VHA’s fiscal year 2021 data, GAO found the rate
at which rural veterans used outpatient care was much lower than urban veterans, with only 21% of rural veterans utilizing these facilities compared to 79% of urban veterans.
What veterans healthcare issues should Congress and the VA prioritize?
The new Congress and policymakers should prioritize proper implementation of the Mission Act, effective veteran suicide prevention initiatives, and improved access to healthcare and benefits.
For the Mission Act, which is aimed at strengthening comprehensive healthcare for veterans, Congress must ensure the VA adheres to the access standards listed in the bill.
More specifically, the VA must:
- expand and increase community care provisions;
- maintain accessibility standards for community care so veterans can receive quality care when the VA cannot provide it in time or within a reasonable distance;
- increase the visibility and better explain VA benefits prior to service members’ military separation;
take a proactive, comprehensive approach to veteran mental health care and support, with well-defined initiatives around suicide prevention; and - reduce wait times for connection to VA providers and right-size VA equities in underserved areas.
There have been a few promising legislative steps since the new Congress took office in January 2023. The VA expanded benefits eligibility to over 3.5 million veterans after the PACT Act was passed in August 2022. The VA also launched a mobile application called VA: Health and Benefits, meant to centralize veterans’ health and benefits information and streamline navigation of VA services.
The Biden administration announced in January that veterans in suicidal crisis can receive free emergency medical care at any VA or private care facility. The AUTO Act was also signed into law in early 2023, allowing disabled veterans who need modified vehicles to receive a grant from the VA every 10 years instead of only once in a lifetime.
Congress should double down on such efforts and focus on the many solvable healthcare challenges veterans are facing. Effective initiatives are needed around veteran suicide prevention, ensuring access to healthcare and benefits, and supporting rural and underserved veteran communities. The serious impact such issues have in the lives of veterans should inspire Congress to prioritize legislation and policies that can address these needs.
How can we assist veterans in getting the healthcare they need?
When looking to assist veterans you know in getting the care they need, you should point them to useful information on VA healthcare benefits and providers. You can also reach out to your Congressional representatives via letters or emails and urge them to prioritize veterans issues, particularly healthcare access.
The veteran community is a vital demographic in America. Their commendable service and sacrifice continue to benefit our nation. As such, they deserve more efficiency in the healthcare they utilize and proper mental health support.
Mission Roll Call (MRC) is committed to furthering our advocacy efforts around healthcare access on behalf of veterans across the country. We take a bipartisan approach to encourage leaders in Washington to consider the everyday needs of veterans in their decision-making.
We educate and inform our members on helpful resources as well. To that end, we’ve partnered with organizations such as America’s Warrior Partnership, Patriot Paws, Panhandle Warrior Partnership, Black Ops Rescue, Sierra Delta, Higher Ground, Camp Southern Ground, and Boulder Crest Foundation.
MRC will continue to advocate for these objectives through outreach, polling, and the media. It’s essential that our country ensures veterans are aware of the benefits available to them and that they can access quality care with relative ease. We can all play a part by speaking up about veterans healthcare issues in our networks and spheres of influence.